All published articles of this journal are available on ScienceDirect.
Content Validity of the Comprehensive ICF Core Set for Chronic Obstructive Pulmonary Diseases: An International Delphi Survey
Abstract
Introduction:
The “Comprehensive ICF Core Set for Chronic Obstructive Pulmonary Diseases (COPD)“ is an application of the International Classification of Functioning, Disability and Health (ICF) and represents the typical spectrum of problems in functioning of patients with COPD. The objective of this study was to validate this ICF Core Set from the perspective of physicians.
Materials and Methodology:
Physicians experienced in COPD treatment were asked about the patients’ problems treated by physicians in patients with COPD in a three-round electronic mail survey using the Delphi technique. Responses were linked to the ICF.
Results:
Seventy-six physicians in 44 countries gave a total of 1330 responses that were linked to 148 different ICF categories. Nine ICF categories were not represented in the Comprehensive ICF Core Set for COPD although at least 75% of the participants have rated them as important. Nineteen concepts were linked to the not yet developed ICF component personal factors and seventeen concepts were not covered by the ICF.
Conclusion:
The high percentage of ICF categories represented in the ICF Core Set for COPD indicates satisfactory content validity from the perspective of the physicians. However, some issues were raised that were not covered and need to be investigated further.
INTRODUCTION
Chronic obstructive pulmonary diseases (COPD), as defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD), are characterized by airflow obstruction that is no longer fully reversible and is usually progressive. [1-3]. COPD often leads to limitations of physical activities and restrictions in daily activities and societal participation [4,5]. Furthermore, psychological problems like anxiety and depression are common [6].
To optimize interventions aimed at maintaining functioning and minimizing disability, a proper understanding of these limitations of the patients’ functioning is needed [7]. The World Health Organization International Classification of Functioning, Disability and Health (ICF) offers a useful framework for classifying the components of health and consequences of a disease. It aims at providing a unified language for the description of health conditions in rehabilitation and a common framework for all health professions [8]. According to the ICF, the problems associated with a disease may concern body functions and structures, the performance of activities and participation in life situations. Health states and the development of disability are modified by contextual factors such as environmental and personal factors [8].
The ICF is structured into two parts – Functioning & Disability (Part 1) and Contextual Factors (Part 2). The overall structure of the ICF is shown in Fig. (1). Part 1 covers functioning and disability and includes the components: Body Functions (b), Body Structures (s) and Activities and Participation (d). In contrast to other disability models, the ICF classifies contextual factors (Part 2) that may either facilitate or hinder functioning and therefore affect the development of disability. These contextual factors consist of two components. The component Environmental Factors (e) encompasses categories of the physical, social or attitudinal world. The second component is Personal Factors (pf) that include gender, age, habits, lifestyle, coping style, etc. ‘Personal factors’ are not yet contained in the current ICF version.

Structure of the International Classification of Functioning, Disability and Health (with permission of the World Health Organization (WHO). All rights are reserved by the WHO)
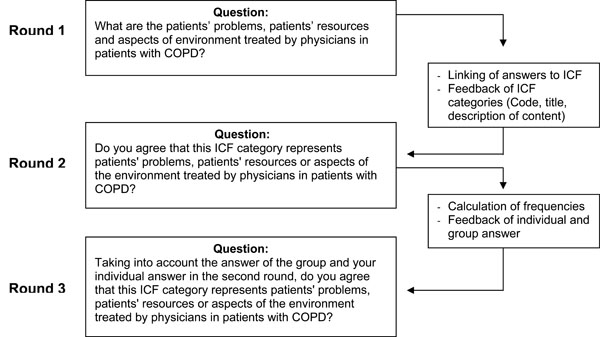
Description of the Delphi process.
Categories are the units of the ICF classification. They are arranged in a stem-branch-leaf scheme, so that a lower-level category shares the attributes of the higher level of which it is a member. For further information on the conceptual background, underlying definitions and structure of the ICF, we refer to the respective WHO publication [8].
Despite its supposed value, the ICF as a whole - including more than 1400 categories - is not feasible for use in clinical practice. In order to facilitate the implementation of the ICF into clinical practice, ICF Core Sets for a number of health conditions including COPD [9], have been developed [10]. The Comprehensive ICF Core Set for COPD includes a set of categories out of the whole ICF, which covers the typical spectrum of problems in functioning in patients with COPD [9]. It was developed in a formal decision-making and consensus process integrating evidence gathered from preliminary studies and expert knowledge [11-13].
While the GOLD definition of COPD does not specifically include patients with chronic bronchitis and emphysema, it is clear that they are considered to be the predominant causes of COPD.
The inclusion of patients with asthma in the ICF Core Sets for COPD was a major challenge at the beginning of the development process [8]. COPD and asthma differ with regard to age, risk factors, course and treatment. However, many symptoms presented by patients do not clearly relate exclusively to either asthma or COPD, and the distinction between these conditions may become quite difficult, especially when COPD is complicated by acute viral or irritant-induced bronchospasm, for example. Therefore it was clearly decided to include asthma under the umbrella term COPD by keeping in mind the need to focus on patients in more severe stages with some degree of fixed airflow obstruction.
Otherwise less common forms of chronic obstructive lung disorders with vastly different etiologies, pathogenesis, symptoms and outcomes, e.g. bronchiectasis, upper-airway lesions, bronchiolar diseases and some interstitial lung diseases, were excluded [9].
The Comprehensive ICF Core Set for COPD is now undergoing worldwide testing and validation using a number of approaches including international multi-centre field studies and validation from the patients’ perspective. One key aspect is the validation from the user perspective. Since ICF Core Sets should serve as a standard for multi-professional assessment and assessment in clinical trials, it is most important whether the categories included in the Comprehensive ICF Core Sets cover the patients’ problems addressed by the specific interventions of health professionals.
Therefore, the objective of this study was to validate the Comprehensive ICF Core Set for COPD from the perspective of physicians. The specific aims were firstly, to identify the patients’ problems, resources and aspects of environment treated by physicians in patients with COPD and secondly, to examine how these aspects are represented by the current version of the Comprehensive ICF Core Sets for COPD.
MATERIALS AND METHODOLOGY
We conducted a three-round electronic-mail survey of physicians using the Delphi technique [14]. The Delphi method is a structured communication technique which aims to gain consensus from a panel of individuals who have knowledge of the topic being investigated [15]. These informed persons are commonly titled as ‘experts’. The experts are requested to complete questionnaires in two or more rounds. Typically, the first round is used to generate ideas and starts with an open question thus allowing participants freedom in their responses. In each of the following rounds, a summary of the previous round is included and evaluated by the participants. The participants are enabled to compare the group results with their own response and are encouraged to revise their answers in light of the replies of other participants. During this process the range of answers is expected to decrease and the group will converge towards a “consensus”. The Delphi process is stopped after a pre-defined criterion (e.g. number of rounds). Besides structured information flow and regular feedback, anonymity of the participants is another key characteristic of the Delphi methods [16]. It provides an equal chance for each participant to present ideas unbiased by other participants. Since the Delphi technique is based on written information and does not require the physical presence of the participants, the method facilitates international, email- or internet-based execution of studies.
Recruitment of Participants
In the preparatory phase of the study, 25 associations for respiratory medicine found by internet search were contacted by e-mail. In addition, literature search and personal recommendations were used to identify experts. Accessorily, a register of members of a German pulmonary specialist association was used to get in contact with German experts. The sample was selected using a purposive sampling approach. Purposive sampling is based on the assumptions that a researcher’s knowledge about the population can be used to handpick the cases to be included in the sample [17].
Lacking a world-wide accepted definition of an ‘expert in respiratory medicine’, the initial letter notes that participants should be “physicians experienced in the treatment of COPD”.
The first contact included an invitation to cooperate and a detailed description of the projects targets, the Delphi process and the timeline. Only persons who agreed to participate were included into the expert sample and received the questionnaire of the first Delphi round.
Delphi Process
The process and verbatim questions of the electronic-mail survey using the Delphi technique are displayed in Fig. (2). The participants had 3 weeks to mail their responses for each round. Reminders were sent one week and 2 days before deadline.
In round 1 of the Delphi survey an information letter including instructions and an Excel file containing an open-ended questionnaire was sent to all experts. In the questionnaire the participants were requested to list all the patients’ problems, patients’ resources and aspects of environment treated by physicians in patients with COPD. Additionally, the participants were asked to complete questions on demographic characteristics and professional experience. Responses were collected and linked to the ICF.
In the second Delphi round, the participants received a list of the ICF categories linked to the responses of the first round. The responses that could not be linked to an existing ICF category were categorized by the research team and listed. The participants were requested to agree or disagree whether the respective ICF category represents patients’ problems, patients’ resources or aspects of environment treated by physicians in patients with COPD.
In the third Delphi round the participants received a list of the ICF categories including the proportion and the identification numbers of the participants who did agree that the categories represent patients’ problems, patients’ resources or aspects of environment treated by physicians in patients with COPD. The participants were requested to answer the same question taking into account the responses of the group as well as their previous response.
Linking
An ICF category is coded by the component letter and a suffix of one to five digits. The letters b, s, d and e refer to the components Body Functions (b), Body Structures (s), Activities and Participation (d) and Environmental Factors (e) (Fig. 1). This letter is followed by a one digit number indicating the chapter, the code for the second level (two digits) and the third and fourth levels (one digit each). A higher-level (more detailed) category shares the lower-level categories of which it is the member, i.e. the use of a higher-level category implies that the lower-level category is applicable, but not the other way round.
Each response of the first Delphi round was linked to the most precise ICF category. The linkage was performed separately by two health professionals on the basis of ten linking rules, established in previous studies [18].
Statistical Methods
Statistical analysis was performed using SAS for windows Version 8. Descriptive statistics were used to characterize the sample and frequencies of responses. Kappa statistics with bootstrapped confidence intervals were used to describe the agreement between the two health professionals who performed the linking [19,20].
RESULTS
Recruitment and Participants
Three hundred thirty seven physicians found by internet search were contacted and 54 of them participated in the first Delphi round. Of the German Association for Pneumology and Respiratory Medicine, 109 members were invited to participate,15 agreed and eight participated in the first round of the study. By literature search, 12 additional experts were contacted and participated in the study. On the basis of personal recommendations of other participants (“snowball system”) 14 persons were contacted. Two of them participated in the first round of the Delphi process.
Seventy-six of 99 physicians (76.8%) who agreed to participate in the study filled in the first round questionnaire. The demographic and professional characteristics of the experts are shown in Table 1.
Attrition of Participants Between the Delphi Rounds, Demographics and Professional Experience of the Round 1 Participants
| WHO-Region | Round 1 (n) | Round 2 (n) | Round 3 (n) | Female (%) | Age Median (Min-Max) | Professional Experience [Years] Median (Min-Max) | OPD Experience [Years] Median (Min-Max) | Self-Rating OPD Expertise# Median (Min-Max) | Mainly Treating Patients in Acute Situation (n) | Mainly Treating Patients in Early-Postacute Situation (n) | Mainly Treating Patients in Chronic Situation (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| African Region1 | 3 | 3 | 3 | 0.0 | 53.0 (49-59) | 20.0 (18-29) | 18.0 (7-24) | 4 (1-4) | 0 | 0 | 3 |
| Region of the Americas2 | 16 | 14 | 13 | 25.0 | 49.5 (36-65) | 20.5 (5-42) | 20.5 (5-31) | 5 (3-5) | 9 | 11 | 16 |
| South-East Asia Region3 | 3 | 3 | 2 | 0.0 | 52.0 (48-56) | 30.0 (20-36) | 26.0 (20-36) | 4 (4-5) | 2 | 2 | 3 |
| European Region4 | 35 | 28 | 27 | 11.4 | 48.0 (37-63) | 20.0 (10-37) | 18.0* (8-35) | 4.5* (3-5) | 24 | 16 | 25 |
| Eastern Mediterranean Region5 | 6 | 5 | 5 | 33.3 | 53.0 (42-59) | 26.5 (15-33) | 18.0 (4-33) | 4.5 (3-5) | 5 | 5 | 6 |
| Western Pacific Region6 | 13 | 12 | 11 | 23.1 | 49.0 (35-66) | 23.0 (10-34) | 20.0 (6-32) | 4 (4-5) | 10 | 10 | 12 |
| Total | 76 | 65 | 61 | 17.1 | 49.0 (35-66) | 21.0 (5-42) | 18.5 (4-36) | 5 (3-5) | 50 | 44 | 65 |
# 1=low 5=excellent
* data of one participant missing
1 Cameroon, Nigeria, South Africa, Sudan
2 Argentina, Canada, Mexico, Peru, Trinidad and Tobago, United States of America, Uruguay
3 India, Republic of Korea, Thailand
4 Austria, Bulgaria, Croatia, Finland, France, Germany, Hungary, Iceland, Italy, Kyrgyzstan, Malta, Norway, Portugal, Russia, Serbia and Montenegro, Slovenia, Switzerland, Turkey
5 Egypt, Iran, Lebanon, Syria, Tunisia
6 Australia, Hong Kong China, Japan, Malaysia, New Zealand, Philippines, Vietnam.
Linking of the Experts Responses to the ICF Categories of the Component Body Functions: The Table Denotes the Percentage of Experts who Considered the Respective ICF Category as Relevant in the Third Delphi Round and the Correlation with the Comprehensive ICF Core Set for COPD. ICF Categories Included Comprehensive ICF Core Set for COPD are Printed in the Bold-Face Type.
| ICF Code | ICF Category Title | Round 3 n=61 | Inclusion in ICF Core Set for COPD | ||
|---|---|---|---|---|---|
| 2nd Level | 3rd Level | 4th Level | |||
| b110 | Consciousness functions | 91.8% | no | ||
| b1263 | Psychic stability | 85.2% | no | ||
| b1265 | Optimism | 80.0% | no | ||
| b1266 | Confidence | 65.5% | no | ||
| b130 | Energy and drive functions | ||||
| b1300 | Energy level | 66.1% | yes* | ||
| b1301 | Motivation | 76.7% | yes* | ||
| b1302 | Appetite | 65.5% | yes* | ||
| b134 | Sleep functions | 86.4% | yes | ||
| b1342 | Maintenance of sleep | 88.3% | yes* | ||
| b1343 | Quality of sleep | 91.7% | yes* | ||
| b1470 | Psychomotor control | 50.0% | yes* | ||
| b152 | Emotional functions | 46.7% | yes | ||
| b1522 | Range of emotion | 41.7% | yes | ||
| b220 | Sensations associated with the eye and adjoining structures | 29.5% | no | ||
| b280 | Sensation of pain | 85.2% | yes | ||
| b2801 | Pain in body part | ||||
| b28010 | Pain in head and neck | 55.0% | yes* | ||
| b28011 | Pain in chest | 93.4% | yes* | ||
| b310 | Voice functions | ||||
| b3400 | Production of notes | 13.8% | no | ||
| b410 | Heart functions | 93.3% | yes | ||
| b4100 | Heart rate | 95.1% | yes* | ||
| b415 | Blood vessel functions | 80.0% | no | ||
| b420 | Blood pressure functions | 88.1% | no | ||
| b4200 | Increased blood pressure | 91.7% | no | ||
| b430 | Haematological system functions | 91.7% | yes | ||
| b4301 | Oxygen-carrying functions of the blood | 95.0% | yes* | ||
| b435 | Immunological system functions | 93.3% | yes | ||
| b4350 | Immune response | 94.9% | yes* | ||
| b4351 | Hypersensitivity reactions | 93.2% | yes* | ||
| b440 | Respiration functions | 98.3% | yes | ||
| b445 | Respiratory muscle functions | 98.4% | yes | ||
| b450 | Additional respiratory functions | 96.7% | yes | ||
| b455 | Exercise tolerance functions | 100.0% | yes | ||
| b4550 | General physical endurance | 96.6% | yes* | ||
| b4551 | Aerobic capacity | 96.7% | yes* | ||
| b4552 | Fatiguability | 95.1% | yes* | ||
| b460 | Sensations associated with cardiovascular and respiratory functions | 98.4% | yes | ||
| b5104 | Salivation | 36.1% | no | ||
| b5106 | Regurgitation and vomiting | 66.1% | no | ||
| b5153 | Tolerance to food | 34.5% | no | ||
| b530 | Weight maintenance functions | 96.6% | yes | ||
| b540 | General metabolic functions | 67.8% | no | ||
| b545 | Water, mineral and electrolyte balance functions | 94.8% | no | ||
| b5500 | Body temperature | 78.0% | no | ||
| b640 | Sexual functions | 67.2% | no | ||
| b6403 | Functions of sexual resolution phase | 19.0% | no | ||
| b710 | Mobility of joint functions | 57.6% | no | ||
| b730 | Muscle power functions | 70.0% | yes | ||
| b735 | Muscle tone functions | 50.0% | no | ||
| b740 | Muscle endurance functions | 62.1% | yes | ||
| b7651 | Tremor | 62.7% | no | ||
| b780 | Sensations related to muscles and movement functions | ||||
| b7801 | Sensation of muscle spasm | 59.3% | yes* | ||
| b810 | Protective functions of the skin | 48.3% | no | ||
| b820 | Repair functions of the skin | 46.7% | no | ||
* ICF category is represented in the Comprehensive ICF Core Set for COPD by its corresponding higher-level (second or third level) category.
Linking of the Experts Responses to the ICF Categories of the Component Body Structures: The Table Denotes the Percentage of Experts who Considered the Respective ICF Category as Relevant in the Third Delphi Round and the Correlation with the Comprehensive ICF Core Set for COPD. ICF Categories Included Comprehensive ICF Core Set for COPD are Printed in the Bold-Face Type
| ICF Code | ICF Category Title | Round 3 n=61 | Inclusion in ICF Core Set for COPD | ||
|---|---|---|---|---|---|
| 2nd Level | 3rd Level | 4th Level | |||
| s410 | Structure of cardiovascular system | ||||
| s430 | Structure of respiratory system | ||||
| s4301 | Lungs | 98.1% | yes* | ||
| s43011 | Alveoli | 94.0% | yes* | ||
| s710 | Structure of head and neck region | ||||
| s720 | Structure of shoulder region | ||||
| s760 | Structure of trunk | ||||
| s7702 | Muscles | 90.2% | no | ||
* ICF category is represented in the Comprehensive ICF Core Set for COPD by its corresponding higher-level (second or third level) category.
Linking of the Experts Responses to the ICF Categories of the Component Activities and Participation: The Table Denotes the Percentage of Experts who Considered the Respective ICF Category as Relevant in the Third Delphi Round and the Correlation with the Comprehensive ICF Core Set for COPD. ICF Categories Included Comprehensive ICF Core Set for COPD are Printed in the Bold-Face Type
| ICF Code | ICF Category Title | Round 3 n=61 | Inclusion in ICF Core Set for COPD | ||
|---|---|---|---|---|---|
| 2nd Level | 3rd Level | 4th Level | |||
| d230 | Carrying out daily routine | 61.0% | yes | ||
| d240 | Handling stress and other psychological demand | ||||
| d330 | Speaking | 23.3% | yes | ||
| d410 | Changing basic body position | 53.3% | yes | ||
| d4100 | Lying down | 41.7% | yes* | ||
| d4153 | Maintaining a sitting position | 33.3% | no | ||
| d4154 | Maintaining a standing position | 43.3% | no | ||
| d430 | Lifting and carrying objects | ||||
| d4301 | Carrying in the hands | 23.3% | yes* | ||
| d4302 | Carrying in the arms | 30.5% | yes* | ||
| d4303 | Carrying on shoulders, hip and back | 27.6% | yes* | ||
| d450 | Walking | 65.0% | yes | ||
| d455 | Moving around | 48.3% | yes | ||
| d4551 | Climbing | 46.7% | yes* | ||
| d460 | Moving around in different locations | 50.8% | yes | ||
| d4601 | Moving around within buildings other than home | 45.8% | yes* | ||
| d4602 | Moving around outside the home and other buildings | 49.2% | yes* | ||
| d470 | Using transportation | 39.0% | yes | ||
| d4702 | Using public motorized transportation | 44.1% | yes* | ||
| d475 | Driving | ||||
| d4750 | Driving human-powered transportation | ||||
| d4751 | Driving motorized vehicles | 32.2% | yes* | ||
| d510 | Washing oneself | 48.3% | yes | ||
| d5101 | Washing whole body | 47.5% | yes* | ||
| d5202 | Caring for hair | 28.8% | no | ||
| d540 | Dressing | ||||
| d570 | Looking after one’s health | ||||
| d5701 | Managing diet and fitness | 71.7% | yes* | ||
| d5702 | Maintaining one's health | 88.3% | yes* | ||
| d610 | Acquiring a place to live | 20.7% | no | ||
| d620 | Acquisition of goods and services | ||||
| d6200 | Shopping | 25.9% | yes* | ||
| d630 | Preparing meals | 28.6% | no | ||
| d640 | Doing housework | 31.0% | yes | ||
| d6400 | Washing and drying clothes and garments | 22.4% | yes* | ||
| d6401 | Cleaning cooking area and utensils | 25.4% | yes* | ||
| d6402 | Cleaning living area | 28.8% | yes* | ||
| d650 | Caring for household objects | 22.0% | yes | ||
| d660 | Assisting others | ||||
| d740 | Formal relationships | 23.7% | no | ||
| d7400 | Relating with persons in authority | 21.1% | no | ||
| d7500 | Informal relationships with friends | 20.3% | no | ||
| d760 | Family relationships | 37.3% | no | ||
| d770 | Intimate relationships | ||||
| d7702 | Sexual relationships | 45.6% | yes* | ||
| d820 | School education | 13.6% | no | ||
| d845 | Acquiring, keeping and terminating a job | ||||
| d8450 | Seeking employment | 37.3% | yes* | ||
| d8451 | Maintaining a job | 49.2% | yes* | ||
| d8452 | Terminating a job | 43.3% | yes* | ||
| d850 | Remunerative employment | 27.1% | yes | ||
| d855 | Non-remunerative employment | 15.3% | no | ||
| d8700 | Personal economic resources | 21.1% | no | ||
| d910 | Community life | ||||
| d9100 | Informal associations | 20.3% | yes* | ||
| d9101 | Formal associations | 13.6% | yes* | ||
| d920 | Recreation and leisure | 53.3% | yes | ||
| d9200 | Play | 26.7% | yes* | ||
| d9201 | Sports | 41.7% | yes* | ||
| d9202 | Arts and culture | 18.3% | yes* | ||
| d9204 | Hobbies | 21.7% | yes* | ||
| d9205 | Socializing | 25.4% | yes* | ||
* ICF category is represented in the Comprehensive ICF Core Set for COPD by its corresponding higher-level (second or third level) category.
Linking of the Experts Responses to the ICF Categories of the Component Environmental Factors: The Table Denotes the Percentage of Experts who Considered the Respective ICF Category as Relevant in the Third Delphi Round and the Correlation with the Comprehensive ICF Core Set for COPD. ICF Categories Included Comprehensive ICF Core Set for COPD are Printed in the Bold-Face Type
| ICF Code | ICF Category Title | Round 3 n=61 | Inclusion in ICF Core Set for COPD | ||
|---|---|---|---|---|---|
| 2nd Level | 3rd Level | 4th Level | |||
| e110 | Products or substances for personal consumption | ||||
| e1100 | Food | 57.6% | yes* | ||
| e1101 | Drugs | 86.4% | yes* | ||
| e115 | Products and technology for personal use in daily living | 51.7% | yes | ||
| e1151 | Assistive products and technology for personal use in daily living | 74.1% | yes* | ||
| e120 | Products and technology for personal indoor and outdoor mobility and transportation | ||||
| e135 | Products and technology for employment | 24.6% | no | ||
| e140 | Products and technology for culture, recreation and sport | 24.1% | no | ||
| e150 | Design, construction and building products and technology of buildings for public use | 20.7% | yes | ||
| e155 | Design, construction and building products and technology of buildings for private use | 22.4% | yes | ||
| e1650 | Financial assets | 15.5% | no | ||
| e2200 | Plants | 17.9% | no | ||
| e2201 | Animals | 17.5% | no | ||
| e225 | Climate | 51.7% | yes | ||
| e2250 | Temperature | 67.8% | yes* | ||
| e2251 | Humidity | 64.9% | yes* | ||
| e2252 | Atmospheric pressure | 31.0% | yes* | ||
| e2253 | Precipitation | 27.6% | yes* | ||
| e2254 | Wind | 27.6% | yes* | ||
| e2255 | Seasonal variation | 54.2% | yes* | ||
| e235 | Human-caused events | 22.4% | no | ||
| e245 | Time-related changes | ||||
| e2450 | Day/night cycles | ||||
| e260 | Air quality | 62.7% | yes | ||
| e2600 | Indoor air quality | 86.2% | yes* | ||
| e2601 | Outdoor air quality | 54.4% | yes* | ||
| e310 | Immediate family | 37.9% | yes | ||
| e315 | Extended family | 14.0% | no | ||
| e320 | Friends | ||||
| e340 | Personal care providers and personal assistants | ||||
| e350 | Domesticated animals | 36.8% | no | ||
| e355 | Health professionals | 96.6% | yes | ||
| e410 | Individual attitudes of immediate family members | 50.0% | yes | ||
| e415 | Individual attitudes of extended family members | 29.3% | no | ||
| e420 | Individual attitudes of friends | ||||
| e450 | Individual attitudes of health professionals | 89.7% | yes | ||
| e460 | Societal attitudes | 33.9% | yes | ||
| e465 | Social norms, practices and ideologies | 24.6% | no | ||
| e540 | Transportation services, systems and policies | 27.6% | yes | ||
| e5502 | Legal policies | 16.9% | no | ||
| e555 | Associations and organizational services, systems and policies | ||||
| e5550 | Associations and organizational services | 50.8% | yes* | ||
| e570 | Social security services, systems and policies | 51.7% | no | ||
| e5700 | Social security services | 56.7% | no | ||
| e575 | General social support services, systems and policies | 61.7% | yes | ||
| e5750 | General social support services | 62.7% | yes* | ||
| e580 | Health services, systems and policies | ||||
| e5800 | Health services | 85.0% | yes* | ||
| e5801 | Health systems | 76.7% | yes* | ||
| e5802 | Health policies | 69.0% | yes* | ||
| e585 | Education and training services, systems and policies | ||||
| e590 | Labour and employment services, systems and policies | ||||
* ICF category is represented in the Comprehensive ICF Core Set for COPD by its corresponding higher-level (second or third level) category.
Delphi Process
In the first Delphi round, 1330 patients’ problems, patients’ resources or aspects of environment treated by physicians in patients with COPD were named. Sixty-five of 76 participants (85.5%) returned the second round questionnaire. The third round questionnaire was completed by 61 of 65 (93.8%) participants.
Linking Process
A total of 148 ICF categories were linked to the pulmologists’ responses. Health conditions such as ‘pneumonia’ and ‘respiratory infection’ that were used in many responses as e.g. a substitute or umbrella term for the underlying disease or as an independent risk factor, were assigned Health conditions. Health conditions are classified and coded in the complementary International Classification of Diseases, ICD 10 [21]. The content of the identified 19 responses linked to the ICF component Personal factors, refers to coping strategies, personal wishes, helplessness and dependencies. Seventeen responses were found not to be covered by the ICF, such as oedema, exacerbations and prevention of exacerbations, expectorations, carbon dioxide retention and lung function studies.
The Kappa statistic for the linking was 0.66 with a 95% bootstrapped confidence interval of 0.63 - 0.69.
Representation of the Physicians’ Responses in the Comprehensive ICF Core Set for COPD
All components of the ICF were represented in the participants’ responses. Tables 2-5 show the linking of the experts’ responses to the ICF categories of the four ICF components Body Functions (Table 2), Body Structures (Table 3), Activities and Participation (Table 4) and Environmental Factors (Table 5).
Of the 148 identified ICF categories, nine are not represented in the Comprehensive ICF Core Set for COPD and considered important by at least 75% of the participants (see Tables 2-5). Eight of these ICF categories belong to the ICF component Body Functions (Table 2).
DISCUSSION
This paper recruited physicians experienced in the treatment of COPD by contacting national and international associations for respiratory medicine, conducted a three-round electronic-mail survey of physicians using the Delphi technique, examined the content by linking the concepts to the ICF and generated an inventory which shows the extent to which the patients’ problems, resources and environmental factors treated by physicians are represented in the Comprehensive ICF Core Set for COPD. Lacking a universal definition of an appropriate level of consensus and based on previous studies, an agreement of at least 75% among the physicians in the final Delphi round was considered sufficiently high [10, 22]. Consequently, ICF categories with an agreement of at least 75%, which are not represented in the Comprehensive ICF Core Set for COPD may indicate missing content validity from the perspective of physicians.
By linking all responses it could be shown that the Comprehensive ICF Core Set for COPD is a valid tool with few exceptions. A total of 148 categories were used to map the contents of the pulmologists’ responses. The finding that the content of only nine categories is not covered by the current Comprehensive ICF Core Set for COPD supports its comprehensiveness and content validity.
However, it is interesting to note that eight of these nine ICF categories cover contents within the component Body Functions. Considering Body Functions are the key focus of most physicians acting in respiratory medicine, this is not surprising.
Most participants agreed that the ICF category b110 Consciousness functions represents a problem in patients with COPD. Patients with advanced COPD are prone to acute and or chronic respiratory failure, resulting in hospital admission. Clinically, an impairment of the lung as gas exchanger often results in an altered level of consciousness, being a key factor for initiating and maintaining a non-invasive positive pressure ventilation (NPPV) [23]. Thus, from the perspective of physicians, an inclusion of this category in the Comprehensive ICF Core Set for COPD is most important.
The categories b1263 Psychic stability and b1265 Optimism are not included in the Comprehensive ICF Core Set for COPD, but were considered important by the participants. Emotional disorders including depressive symptoms and episodes as well as fears have been found to be very common [6, 24, 25]. Therefore, depression and anxiety are key treatment targets e.g. in pulmonary rehabilitation settings. However, these problems are already sufficiently represented in the Comprehensive ICF Core Set for COPD by the ICF category b152 Emotional functions.
Many participants agreed on the ICF categories b420 Blood vessel functions and b415 Blood pressure functions with respect to pulmonary arterial hypertension (PAH). Since all PAH results in similar histological remodeling of pulmonary arteries with thickening of the intima, proliferation of the media and plexogenic lesions [26], the ICF category s410 Structure of cardiovascular system was included in the ICF Core Set for COPD [9]. In COPD supplemental oxygen and anticoagulation and not vasodilators remain to date the primary treatment for PAH [27]. Its potential reversibility might be explained by restoring blood vessel functions and blood pressure functions. Therefore it might be consequential to include this additional categories (b415 Blood vessel functions, b420 Blood pressure functions and b4200 Increased blood pressure) in the Comprehensive ICF Core Set for COPD.
The ICF category b545 Water, mineral and electrolyte balance functions is not included in the Comprehensive ICF Core Sets for COPD, but was considered as a relevant problem treated by physicians in patients with COPD. Salt and water retention, reduced renal blood flow and diminished glomerular filtration rate as well as neurohumoral-abnormalities [28, 29] can be found in COPD patients. Even though there is only few data available concerning the fluid homeostasis in patients with COPD only, not affected by cardiac co-morbitities e.g. heart failure. However, since sodium retention and resulting volume congestion often lead to massive edema, a common problem of patients with COPD, it may therefore be useful to integrate the ICF category b545 Water, mineral and electrolyte balance functions into the Comprehensive ICF Core Sets for COPD.
Seventy-eight percent of the experts regarded the ICF category b5500 Body temperature as a relevant aspect in patients with COPD, especially in association with acute exacerbations. Unfortunately, many definitions of exacerbations of COPD exists. The most widely used criteria include worsening of dyspnea and changes in sputum production, but not body temperature. Therefore, this category is not included in the Comprehensive ICF Core Set for COPD. However, acute exacerbations of COPD can be characterized by systemic clinical descriptors such as increased body temperature [30, 31]. With regard to diagnostics of exacerbations, one could consider an inclusion of the ICF category b5500 Body temperature in the ICF Core Sets for COPD.
From the ICF component Body Structures, the category s7702 Muscles is not included in the Comprehensive ICF Core Set for COPD, but received an agreement of above 75%. In fact, the ICF categories s710 Structure of head and neck region, s720 Structure of shoulder region and s760 Structure of trunk, which are included in the Comprehensive Core Sets for COPD, also comprise muscles of the respective region. However, since muscle weakness in chronic COPD concerns respiratory muscles as well as limb muscles [32], one should consider whether it could be helpful to include the category s7702 Muscles which focuses on musculo-skeletal structures related to movement.
A large number of the participants’ responses were identified as Personal Factors. Personal factors are contextual factors that relate to the individual such as age, gender, education, coping styles, overall behaviour pattern, character style and individual psychological assets [8]. However, they are not yet classified in the ICF. There is a consensus in literature that personal factors like coping styles, self-efficacy, and optimistic attitude, contribute to medical treatment and quality of life in patients with COPD [33, 34]. It may therefore be helpful to provide a classification of the personal factors in the future to enable a systematic identification of all personal factors influencing the functioning of a certain person.
The Delphi technique was an appropriate method for this study objective. In contrast to the mean attrition rates of 50% or higher from round to round reported in literature, response rates between the rounds ranging from 77 to 94 % were achieved in our study [35, 36].
However, there are some limitations regarding the external validity of this study. First, a small proportion of the physicians who were initially contacted, finally participated in the study. Thus, a selection bias cannot be excluded. Moreover, participants provided a self-rating of their experience with COPD treatment. Although they reported a high median level of experience, objective ratings may have differed from the self-reports. In addition, cultural differences may exist: an expert on COPD in a developing country such as Sudan is expected to have a different level of expertise than a physician from an industrialized country. The overall response rate in this study is similar with studies using comparable strategies to recruit physicians worldwide for a Delphi survey on the ICF [37]. Reasons for not responding to our invitation could have been a lack of interest in rehabilitation issues among the physicians, a low knowledge of the ICF and restricted time resources. However, we were not able to systematically collect information on the reasons for non-responding.
Although the authors were successful in recruiting 76 physicians from 44 countries, the sample consists predominantly of physicians from Europe. Especially from the African, South East Asian and Eastern Mediterranean world region, only few physicians could be recruited. Language barriers as well as a lack of internet access could have influenced the participation, as the Delphi survey was exclusively conducted in English language by electronic mail. Therefore, this sample does not represent the whole spectrum of physicians experienced in the treatment of COPD patients worldwide. In addition, the unequal contribution of countries may also have affected the study results since patients symptoms and functional limitations, and physicians treatment goals may vary between the different cultures. Further validation studies including physicians from countries not sufficiently represented in this study should be conducted.
Another limitation refers to the 75% definition of level of consensus. This level of consensus is within the range of 51% to 80% agreement recommended in the literature [22] and its selection was based on the experiences with the development of ICF Core Sets for chronic conditions [10]. However, a modification of the level of consensus would have affected the results.
CONCLUSION
Although minor shortcomings of the current version of the Comprehensive ICF Core Set for COPD concerning the representation of several body functions and the personal factors from the physicians’ perspective could be detected in this study, the Comprehensive ICF Core Set for COPD can be applied as a useful tool in clinical practice to enhance communication within multi-professional teams by referring to the common framework of the ICF model [8]. Based on the Comprehensive ICF Core Set for COPD, the impairments in body functions and structures, limitations in activities, restrictions in participation and the influential environmental factors of a determined patient can be described and the impact of COPD can be measured in a standardized way. A functioning profile can be created and used as a reference for follow-up. Since the treatment of COPD also requires a coordinated longitudinal care involving several health professions, an approach that structures the management among the different health professionals involved is needed. The Rehab-CYCLE is a problem solving approach for ICF-based rehabilitation management and facilitates goal setting, assignment of intervention targets to specific interventions and responsible health professionals and evaluation of goal achievement [38,39]. The Comprehensive ICF Core Set for COPD can be integrated in the Rehab-CYCLE and provide a useful tool for rehabilitation management.
Further research is necessary regarding the feasibility of the Comprehensive ICF Core Set for COPD in clinical practice. In addition, results of ongoing validation projects will further elucidate the validity of the Comprehensive ICF Core Set for COPD from the perspective of different health professions. The findings of all validation studies could be the basis for a revision and improvement of the Comprehensive ICF Core Set for COPD.
ACKNOWLEDGEMENTS
We thank the participants of the Delphi exercise for their valuable contribution and their time in responding to the demanding questionnaires. In addition, we are grateful to Edda Amann for performing the linking of the participants’ responses to the ICF.
DISCLOSURE
The methodology used to collect the data presented in this paper is very similar to that of a paper previously published in Psychology and Health, Volume 23, Number 6, August 2008, pp. 639-659(21): Thus, there is some overlapping in the information contained in both papers.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.


