All published articles of this journal are available on ScienceDirect.
Respiratory Candida in Patients with Bronchitis, Mucus Plugging, and Atelectasis
Abstract
Background:
The significance of Candida in pulmonary secretions is unclear, and usually is regarded as colonization, not contributing to symptoms or disease. Yet, in our experience, Candida seemed associated with chronic sputum, mucus plugging, atelectasis, and poor outcome.
Objective:
The aim of this study is to describe the clinical findings of patients with Candida in pulmonary (sputum or bronchoscopy) secretions and the significance of Candida.
Methods:
Retrospective study of inpatients and outpatients referred for pulmonary consultation with Candida in pulmonary secretions. Clinical parameters and estimates of whether Candida was likely clinically significant, were determined.
Results:
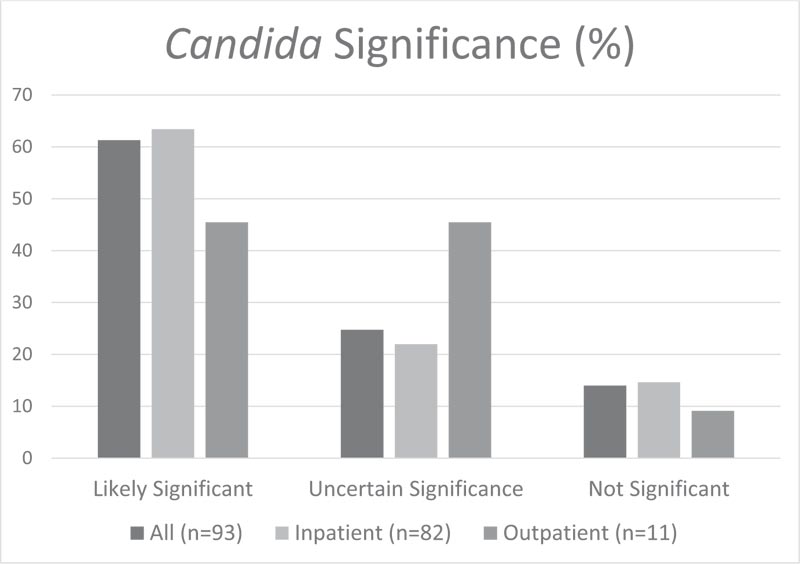
82 inpatients and 11 outpatients were identified, of which 61 (66%) had atelectasis and 68 (73%) bronchoscopies. Of patients having bronchoscopies, 56 (82%) had mucus, and 43 (63%) mucus plugging. Of the inpatients death (or probable death) occurred in 43 (63%), 42 (98%) of which were from definite or probable respiratory failure, with 13 (31%) likely related to mucus plugging, 16 (38%) possibly from mucus plugging, 6 (14%) unknown, and 7 (17%) not due to mucus plugging. Candida was felt likely clinically significant in 57 patients (61%), uncertain significance in 23 (25%), and not significant in 13 (14%). All outpatients had exacerbations, including 7 (64%) within a year.
Conclusion:
Patients requiring pulmonary consultation with Candida in pulmonary secretions often have chronic sputum production, exacerbations, mucus plugging, atelectasis, and death from respiratory failure. Candida was likely clinically significant in most patients. Recommendations to consider Candida in pulmonary secretions as colonization should be reconsidered.
1. INTRODUCTION
The role of Candida in sputum culture is unclear and is generally not treated when present in pulmonary (sputum or bronchoscopy) samples. In cystic fibrosis patients, chronic respiratory colonization of C albicans is associated with worsening pulmonary status [1, 2]. A case series of patients in a long-term acute care hospital with chronic Candida tracheo-bronchitis suggests clinical improvement with antifungal treatment [3]. Treatment recommendations from the Infectious Disease Society of America do not support treatment for Candida in pulmonary secretions [4], with Candida regarded as colonization.
However, our experience suggested that in patients with chronic bronchitis and/or mucus plugging with atelectasis Candida may be clinically significant and/or a marker of poor clinical outcome. We are unaware of any studies reporting the prevalence of Candida in pulmonary secretions among patients with atelectasis or chronic bronchitis, nor attempting to determine whether the Candida is clinically significant.
This retrospective study was performed to describe the clinical status and course of inpatients and outpatients referred for pulmonary evaluation who had Candida in sputum or bronchoscopy samples, and to evaluate whether the Candida was likely clinically significant.
2. METHODS
This is a retrospective study of consecutive patients referred for outpatient or inpatient pulmonary consultation between 8/12/2012 and 9/1/2016 to one of the authors (DJ) at Baystate Medical Center, a 714-bed teaching hospital in Western Massachusetts, and found to have Candida species in their pulmonary secretions, either in sputum or deep respiratory specimens. Patients under age 18 or with cystic fibrosis were excluded. The author (DJ) only sent sputum for fungal culture if there was persisting sputum following at least one course of antibiotics. The electronic medical record was reviewed and information stored using RedCap. The Baystate Health institutional review board approved the study.
Baseline data at initial evaluation or initial identification of Candida if that was later included demographics (age, sex, ethnicity), diagnoses, Xray findings, date of hospitalization when pulmonary consultation occurred, and date of pulmonary consultation. The electronic medical record was searched through 9/1/2017 to determine clinical parameters, antibiotic or antifungal treatment, sputum and bronchoscopy bacterial and fungal culture results, Xray findings, bronchoscopy findings, steroid use, time to exacerbation, date of death, and likely cause of death.
Most bronchoscopies were performed by one of the authors (DJ), whose technique in patients with atelectasis and/or mucus plugging included first clearing visible mucus and plugs in airways with suction. If mucus remained, then 5 cc aliquots of 5% acetylcysteine were instilled, followed after about 10 seconds with suctioning, which usually cleared visible mucus. If mucus was still too thick to suction through the bronchoscope channel, suction was applied while pulling the bronchoscope out of the airways (with mucus on the end of scope), and then the suction channel was cleared with saline. Once visible mucus was cleared from the airways, the bronchoscope was wedged in segments, which had mucus plugs or atelectasis on chest imaging. Then 5 cc of 5% acetylcysteine followed by 10 cc saline was given to segments with mucus plugs or atelectasis followed after about 10 seconds with suctioning, which usually cleared numerous medium then small mucus plugs. This was repeated until no further plugs were cleared. This method usually resulted in the re-inflation of the atelectatic lung. However, many patients redeveloped atelectasis and needed subsequent bronchoscopies. Some patients had air insufflation performed after clearing mucus/plugs on a subsequent bronchoscopy. Air insufflation was performed by wedging the bronchoscope in the atelectatic segment and inflating the segment to 40 cm H2O for about 30 seconds using an Ambu-bag connected to a Montgomery T connector, slip-tip 10 ml syringe, and manometer.
Time to first pulmonary exacerbation was determined from the time between discharge from the hospital or time from outpatient visit to the first exacerbation after finding Candida. Pulmonary exacerbation was defined as either 1) unscheduled physician contact for worsening dyspnea, cough, increased sputum production or change in sputum color or 2) electronic documentation of a new prescription or dosage increase of systemic steroids or a new prescription for an antibiotic.
The significance of positive respiratory culture for Candida was assigned to 3 categories.
(1) Likely clinically significant- if there was any of:
(a) sputum persisting more than a week following antibiotics, or poorly controlled asthma/COPD requiring 10 mg or more prednisone for over 3 weeks following a course of antibiotics
(b) chest imaging consistent with mucus plugging/atelectasis with either Candida without bacteria on at least one bronchoscopy sample or Candida from two samples (bronchoscopy and/or sputum) at least 3 days apart
(c) bronchoscopy consistent with significant airway Candida;
(2) Uncertain significance- with chest imaging consistent with mucus plugging/atelectasis, but Candida on only one sputum or bronchoscopy sample and not having Candida without bacteria on bronchoscopy.
(3) Not significant- if there was neither (1) nor (2) – i.e., no persistent sputum following antibiotics and not mucus plugging/atelectasis on chest imaging.
Probable death was defined as a patient without follow-up in the electronic medical record who was discharged from the hospital with comfort measures only status or transfer to another facility with a severe medical condition expected to worsen.
Data Analysis: For continuous data, mean, standard deviation and ranges were determined. For categorical data, frequencies and percentages were determined.
3. RESULTS
Ninety-three patients were identified with Candida in pulmonary secretions, including 45 males, 48 females, with mean age of 66.2 ± 15.8 years. There were 75 white, 11 Hispanic, 5 black, and 2 Asian. Eighty-two (88%) were initially seen in the hospital and 11 (12%) as outpatients. Many of the inpatients were in intermediate care units, which could manage tracheostomy patients on ventilators, but other physicians managed patients in the medical ICU. Seventy-seven (83%) had initial identification of Candida while they were in the hospital, and 16 (17%) while they were outpatient. Diagnoses included 36 with COPD, 23 asthma, 13 with a tracheostomy, 12 chronic kidney disease, 12 congestive heart failure, and 7 paraplegia.
Most patients received inhaled and/or systemic steroids at some point. 30 (32%) had both inhaled and systemic steroids, 21 (23%) just inhaled steroids, 11 (12%) just systemic steroids, and 31 (33%) had neither. All patients received antibiotics, often numerous courses.
Chest imaging found bronchiectasis in 17 (18%) patients and emphysema in 17 (18%) patients, with 3 patients having both bronchiectasis and emphysema. Atelectasis was common, with initial imaging finding atelectasis in 48 (52%) patients (2 (4%) subsegmental, 3 (6%) segmental, 36 (75%) lobar, and 7 (15%) entire lung). Sixty-one (66%) patients had atelectasis at some point, with greatest atelectasis including 3 (5%) subsegmental, 7 (12%) segmental, 43 (71%) lobar, and 8 (13%) entire lung. Atelectasis was common on patient’s final imaging, being present in 51 patients (55%) (6 (12%) subsegmental, 11 (22%) segmental, 29 (57%) lobar, and 5 (10%) entire lung).
From sputum cultures, 29 (31%) patients had C albicans, including 3 also with C glabrata. Four (4%) patients had Candida non-albicans species (1 C parapsilosis,1 C pseudotropicalis (C kefyr) and C parapsilosis, 1 C tropicalis and C glabrata, 1 C lusitaniae). An additional 8 (9%) patients had ”No Cryptococcus” report on sputum fungal culture, which was likely C albicans or other C. species as the hospital laboratory reported “No Cryptococcus” if there was Candida on sputum culture and the physician did not request further identification soon after the final report. Seven (8%) additional patients had yeast seen on the gram or fungal stain, which was not cultured, again most likely a C species. Thus, Candida was present on sputum samples in 48 (52%) patients.
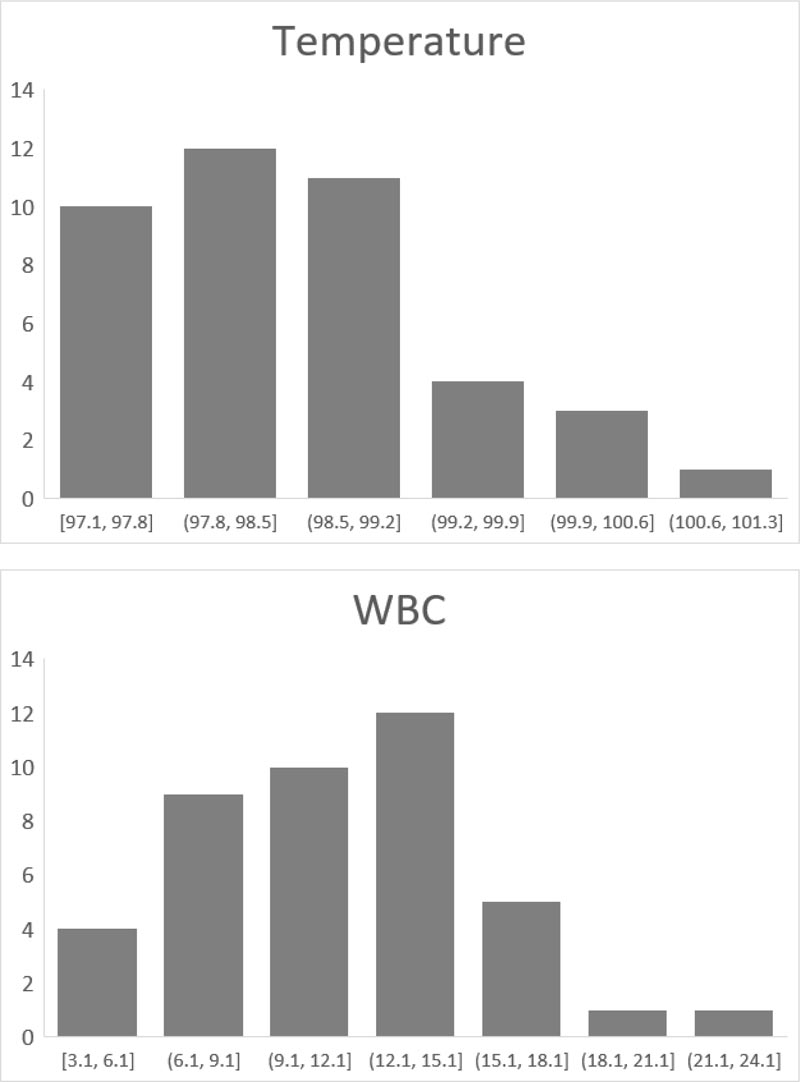
Sixty-eight (73%) patients had bronchoscopies, including 66 (71%) initially seen as inpatients and 2 (2%) as outpatients, with the most common reason being to manage atelectasis. There were no patients who had C species on sputum culture whose bronchoscopy was negative for C species. Forty-nine (53% of all patients, 72% of those with bronchoscopies) patients had at least one bronchoscopy with Candida and negative bacterial culture. At the time of the 49 first bronchoscopies with Candida and negative bacterial culture, 2 patients (4%) had fever (temperature > 100.9) and 20 (41%) leukocytosis (WBC > 10.9) (Fig. 1). Two of the 11 patients initially seen as outpatients had outpatient bronchoscopies.
The 68 (73%) patients had a total of 239 bronchoscopies, with many patients needing multiple bronchoscopies to treat mucus plugging/atelectasis. Twenty-five patients had one bronchoscopy, 16 two, 5 three, 7 four, 2 five, 3 six, 5 seven, 1 eight, 1 nine, 1 fifteen, 1 seventeen, and 1 twenty-seven. Of the outpatients, one had one bronchoscopy and another two.
Findings on the 68 (73%) patients who had bronchoscopy included 6 (9%) without mucus and 19 (28%) without mucus plugging on any bronchoscopy. Two (3%) patients without mucus had mucus plugging. Of the 62 (67%) patients with mucus, there were 10 (16%) small, 23 (37%) moderate, 29 (47%) large amounts of mucus. Of the 49 (53%) patients with mucus plugging, there were 8 (16%) small, 20 (41%) moderate, 21 (43%) large amounts of mucus plugs. One of the patients with much mucus and plugs also had endobronchial lesions suggesting yeast.
Of the 68 patients with bronchoscopy cultures, 54 (79%) patients had C albicans alone, 7 (10%) C albicans and other Candida species (4 C glabrata, 2 both C glabrata and C parapsilosis, 2 C parapsilosis), and 7 (10%) patients had other Candida species without C albicans (3 C glabrata, 3 C tropicalis, 1 C lusitanaie).
Using the criteria described in the methods section, Candida was felt to be clinically significant in 57 (61%) patients, uncertain significance in 23 (25%) patients, and not significant in 13 (14%) patients. (Fig. 2).
Of the 11 (12%) patients initially seen as an outpatient, all had an exacerbation prior to the end of the study, including 1 within 30 days (d), 1 31-60d, 3 61-90d, 2 91-365d, and 4 > 365d. Four (36%) received antifungal therapy at some point in their course of illness. Ten (91%) were known alive at the end of the study and one presumed dead from respiratory failure.
Of the 82 patients initially seen in the hospital, 6 (7%) died in that hospitalization, including 5 which the death may have been related to mucus plugging. Six (7%) patients died within 31 days of discharge, including 4 which the death may have been related to mucus plugging. Another 9 (11%) were discharged expected to die shortly, including 7 which the death may have been related to mucus plugging. Thus, mucus plugging was felt to be related to the death of 16 of the 21 patients (76%) with definite or likely death during the hospitalization or within 31 days of discharge.
With a follow-up of the 82 patients initially seen in the hospital, 27 (33%) had definitely died by the end of the study. This included 6 deaths during the hospitalization, 6 within 31 days of discharge, and 15 after 30 days following admission. Sixteen (20%) probably died (were discharged comfort measures only or with very severe respiratory status), 35 (43%) were alive, and the status was not known for 15 (18%) patients. Thus, there were 43 (52%) patients with definite or probable death. Death from definite or probable respiratory failure occurred in 42 of the 43 (98%) patients, with 13 of the 42 (31%) felt likely related to mucus plugging, sixteen (38%) possibly from mucus plugging, 6 (14%) unknown, and 7 (17%) from causes not related to mucus plugging.
Relatively few patients received antifungal treatment (primarily fluconazole), with 16 (17%) receiving antifungal as inpatient only, 3 (3%) as inpatient and outpatient, and 10 (11%) only as an outpatient. It is possible some patients received antifungal as an outpatient from other health providers. Few inpatients received long courses of antifungals, and one with persisting Candida despite prolonged antifungal was found resistant to fluconazole.
4. DISCUSSION
Our study shows that among inpatients with chronic respiratory illness and mucus plugging and atelectasis, the culture of Candida in sputum or bronchoscopy samples is associated with poor outcomes. Many patients required repeated bronchoscopies for mucus plugging and atelectasis despite antibiotic therapy, and many patients died from respiratory failure. Pulmonary exacerbations were common among outpatients with Candida in sputum samples. The finding in many patients of persistent Candida in respiratory secretions, mucus and mucus plugging following effective antibiotic treatment of bacteria supports the hypothesis that Candida can contribute to mucus, mucus plugging, and atelectasis, and thus be clinically significant.
The standard of care in interpreting Candida in sputum or bronchoscopy samples is to ignore this as clinically insignificant [4]. It is assumed the Candida represents colonization, i.e., the organism can be found in or on the body, but it is not causing any symptoms or disease [5]. A study of critically ill immunocompetent patients found that checking bronchoscopy samples for fungal culture rarely led to changes in therapy [6]. Isolation of Candida from pulmonary secretions in critically ill mechanically ventilated patients is estimated to be about 50%, while Candida pneumonia is rare in immunocompetent patients [7]. A study of 25 non-neutropenic, mechanically ventilated patients who died found Candida from pulmonary specimens in 40% of patients and Candida pneumonia in 8% [8]. A study of patients with intensive care unit-acquired pneumonia found that Candida was a marker of higher severity, which was found in 21% of patients, and that antifungal treatment did not influence outcomes [9].
While Candida is usually ignored in pulmonary secretions, some studies suggest that Candida may be significant. A study found that respiratory tract Candida “colonization” was associated with pneumonia due to Pseudomonas aeruginosa, a longer duration of mechanical ventilation, and increased length of ICU and hospital stay [10]. Another retrospective study of suspected ventilator-associated pneumonia showed increased hospital stay and mortality (unadjusted OR 2.9 (95% CI 1.6 to 5.2) in those with Candida in the respiratory tract [11]. A case series found improvement with antifungal treatment of chronic Candida tracheobronchitis [3]. In patients with cystic fibrosis, chronic respiratory colonization with C albicans is associated with worsening lung function and frequency of exacerbation [1],
The present study did not address whether antifungal treatment, either endobronchial/inhalational or systemic treatment is helpful in patients with mucus plugging/atelectasis. Relatively few inpatients received antifungals as in-hospital antifungal therapy which was controlled by the infectious disease, usually deemed Candida in sputum and bronchoscopy samples as colonizers. A double-blind study did not support antifungal therapy in patients with suspected ventilator-associated pneumonia and Candida in endotracheal secretions [12].
While C albicans was the most common C species, many patients had other C species, and many had C albicans with other species. Nearly all sputum fungal cultures were initially reported “No Cryptococcus” without identifying C albicans or other C species, as laboratory policy is to not routinely report Candida on sputum samples sent for fungal culture.
Bronchoscopy was usually performed to evaluate and manage patients with atelectasis, with most patients needing more than one bronchoscopy. Most patients had Candida without bacteria on at least one bronchoscopy, suggesting that Candida is associated with and may contribute to persistent/recurring atelectasis.
It is unknown if Candida can cause chronic airway inflammation that may lead to more respiratory secretions and mucus plugging. There are some similarities between Candida and Aspergillus in the respiratory tract. Both are fungal organisms and are associated with airway “colonization” without evidence of pneumonia or lung parenchymal invasion. Aspergillus can cause ABPA (allergic bronchopulmonary aspergillosis) [13] in which the airway “colonization” leads to an immune response often with increased airways reactivity, bronchiectasis, and high-attenuation mucus plugging. Conceivably, Candida airway “colonization” can trigger similar immune responses associated with increased mucus and large airway mucus plugging and/or atelectasis. Interestingly, steroids are the mainstay of treating ABPA, but steroid use can predispose to Candida. In the current study, 67% of the patients received inhaled and/or systemic steroids.
The bacterial microbiota may be key to Candida's relative virulence. Chronic and multiple uses of antibiotics can affect the indigenous respiratory flora and, thus, play a role in the clinical significance of Candida. The budding yeast and the filamentous hyphal forms of Candida may play a role in the relative virulence of this organism, the latter having more adherence properties. Animal studies suggest a possible direct role of Candida in the disease pathogenesis, with Candida working in synergy with bacteria causing respiratory disease [14]. Candida possibly contributes to excessive mucus production as it is associated with increased levels of TNF-alpha and IFN-gamma within the lung, even in the histological absence of acute infection [14].
CONCLUSION
In conclusion, many patients referred for pulmonary consultation who had Candida in pulmonary secretions have chronic sputum production, exacerbations, mucus plugging, atelectasis, and death from respiratory failure possibly related to the mucus plugging and atelectasis. Using criteria including persisting Candida and Candida without bacteria on bronchoscopy samples, Candida was felt to be clinically significant in the majority of such patients. We agree with a recent review of Candida in the respiratory tract [15], which concludes, “The final word on Candida’s significance in the respiratory tract has yet to be spoken.” Further study is needed to determine whether effective antifungal treatment (combined with clearing mucus and mucus plugs and antibiotics, if also bacterial infection) improves patient outcomes in such patients.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Baystate Health Institutional Review Board approved the study.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
There was no patient consent required, due to retrospective nature of the study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


