All published articles of this journal are available on ScienceDirect.
Factors Associated with Suboptimal Control of Asthma among Adult Asthma Patients: A Cross-sectional Study
Abstract
Introduction:
Asthma is a major public health problem that negatively impacts patients, families, and the community. Identifying risk factors for poor asthma control may greatly enhance the establishment of more effective treatment of asthma. The level of asthma control and risk factors for poor asthma control is relatively unknown in Ethiopia.
Methods:
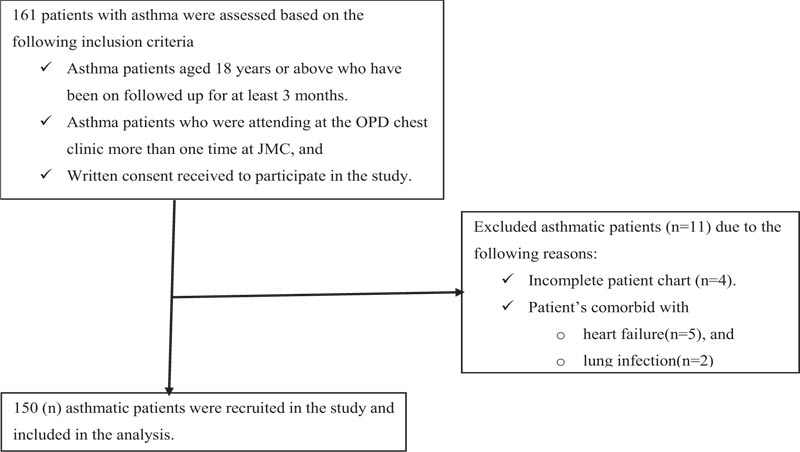
A cross-sectional study was conducted on 150 adult asthma patients at the Outpatient Department (OPD) chest clinic of Jimma Medical Center (JMC), from February 15 –March 20, 2019. The Statistical Package for Social Science (SPSS) 21.0 was used for data analysis. Multivariate logistic regression was conducted to analyze the potential associated factors of suboptimal control of asthma.
Results and Discussion:
Of 150 adults diagnosed with asthma recruited in this study, 81 [54.0%] of them were females, and the mean age of the patients was 41.1 ± 12.4 years. Inhaled corticosteroid (ICS) plus short-acting beta-agonist (SABA) (64, 42.7%) was the most frequently used anti-asthmatic medication. Over one-fourth (26.0%) (95% CI, 19.2-33.8) of study participants had suboptimal asthma control. On multivariate logistic regression, being an urban dweller (AOR=3.70, p=0.025) and not applying proper inhalation technique (AOR=16.23, p=0.022) were increased the risk of suboptimal asthma control, while non-prescription anti-asthmatic drugs taking habit (AOR=0.25, p=0.010) reduces the odds of having suboptimal asthma control.
Conclusion:
Suboptimal asthma control is high among adult asthma patients. Being an urban dweller and not applying proper inhalation techniques were increased the likelihood of suboptimal asthma control, while non-prescription anti-asthmatic drugs taking habits had lower odds of suboptimal asthma control. The authors recommend large sample size studies on the comparative status of asthma control using prescription versus non-prescription anti-asthmatic medication.
1. INTRODUCTION
World Health Organization (WHO) defines asthma as one of the major non-communicable diseases. It is a chronic disease of the air passages of the lungs, which inflames and narrows them [1]. It is characterized by a history of respiratory symptoms, such as wheeze, shortness of breath, chest tightness, and cough that vary over time and intensity, together with variable expiratory airflow limitation [2]. The strongest risk factors for developing asthma are a combination of genetic predisposition with environmental exposure to inhaled substances and particles that may provoke allergic reactions or irritate the airways [1]. Global Initiative for Asthma (GINA) guidelines classified asthma into four categories based on disease severity: mild intermittent, mild persistent, moderate persistent, and severe persistent [2].
The Global Burden of Disease collaboration estimated that 420,000 people in the world died from asthma each year, i.e., more than 1000 per day [3]. Of this, over 80.0% of asthma-related deaths, as well as severe cases, occur in low and middle-income countries [1, 3]. Globally, asthma is ranked 16th among the leading causes of years lived with disability and 28th among the leading causes of the burden of disease, as measured by disability-adjusted life years (DALYs). It accounts for the loss of over 15 million DALYs annually [4].
In Africa, the prevalence of asthma increased across all age groups; it accounted for 49.7 million (13.9%; 95% CI 9.6-18.3) among children <15 years, 102.9 million (13.8%; 95% CI 6.2-21.4) among people aged <45 years, and 119.3 million (12.8%; 95% CI 8.2-17.1) in the total population in 2010 [5]. In Ethiopia, the overall prevalence rate of asthma was 9.1% [6], and it is the 10th Environmental burden by disease category [DALYs/1000 capita] per year with a rate of 1.2 [7].
Overall, asthma is a major public health problem that negatively impacts patients, their families, and the community by inducing work and school loss, poor quality of life, frequent emergency visits, hospitalizations, death [8] as well as increased health care expenditures that can include costs of office visits, hospitalizations, emergency room visits, tests, and medications [4].
Asthma is considered under good control when patients can avoid troublesome symptoms during the day and night, need little or no reliever medication, have a productive and physically active life, have normal or near-normal lung function, avoid serious asthma flare-ups (exacerbations or attacks) [2]. The control of asthma symptoms is a realistic goal, and studies have shown that achieving this in most asthma patients leads to a higher quality of life. Despite this, the control of asthma is generally poor [9]. European-wide, population-based surveys reported prevalence rates of unsatisfactory asthma control levels ranging from 56.6% [10] to 80.0% [11, 12].
Despite WHO's putting an objective on surveillance to map the magnitude of asthma and analyze its determinants of outcome [1], studies are still not sufficient, particularly in low-income countries [13]. Identifying risk factors for poor asthma control may greatly modify adverse effects and potentially lessen the financial burden of the disease. The level of asthma control and risk factors for poor asthma control is relatively unknown in Ethiopia [14]. Therefore, this study aimed to assess factors associated with suboptimal control of asthma among adult asthma patients at the chest clinic of the JMC (Fig. 1).
2. MATERIALS AND METHODS
2.1. Study Design and Setting
A cross-sectional study was conducted at the OPD chest clinic of JMC, a tertiary teaching hospital in Jimma town, Jimma zone, Oromia, South-West Ethiopia. It is located 352 Km from Addis Ababa, the capital. The study was conducted from February 15 –March 20, 2019.
2.2. Sample Size Determination
The required sample size for the study was calculated by using the single population proportion formula by considering 76.1% prevalence of suboptimal asthma control in Ethiopia [14] and considering a 95% confidence level (α= 5%) with ±5% precision (d) and taking the estimated source population of 325 on follow up. The final sample size was 150 adult asthma patients on follow-up at the chest clinic of the JMC.
2.3. Data Collection Procedure and Quality Control
The data abstraction tool was developed to extract important variables by reviewing the patient charts and different kinds of literature that were used to assess the status of asthma control and its associated factors. Data were gathered by a data collector over 34 days (from February 15 –March 20, 2019), from the OPD chest clinic of JMC, from the patients' medical charts, and by interviewing patients for the respective information following a pre-test. The following data were retrieved from the patient medical chart- sex, anti-asthmatic medication, concurrent medication use, and comorbidities. Data extracted from interviewing the patient includes age, residency, educational status, marital status, job-status/category, OPD follow up status, without prescription medication-taking habit, smoking status, living status with a domestic animal, discontinuation of anti-asthmatic medication, the inhalation technique, and response towards assessing the status of asthma control on “daytime symptoms encountered more than twice/week,” “any night waking due to asthma,” “reliever needed more than twice/week,” and “any activity limitation due to asthma.”
2.4. Operational/Term Definitions
The suboptimal asthma control is considered [2] when in the past 4 weeks, has the patient had ≥1 of the following conditions occurred.
- Daytime symptoms more than twice/week.
- Waking up at due to asthma.
- Reliever needed more than twice/week.
- Any activity limitation due to asthma.
2.4.1. Status of Smoking [15, 16]
- Never: An adult who has never smoked, or who has smoked less than 100 cigarettes in his or her lifetime, but who had quit smoking in the last 28 days.
- Former (ex) smoker: An adult who has smoked at least 100 cigarettes in his or her lifetime but who had quit smoking in the last 28 days.
- Current smoker: An adult who has smoked 100 cigarettes in his or her lifetime and has smoked in the last 28 days.
2.4.2. Applying Proper Inhalation Technique
Individuals are assessed on how they use the inhalation technique per the instructions of each device and considered proper if they follow all the procedures of inhalation.
2.4.3. History of Discontinuing Medication
History of the ceasing of anti-asthmatic medication by the patient without the clinician consults.
2.4.4. Non-prescription Anti-asthmatic Medication Taking
Patients taking the anti-asthmatic medication without a doctor's prescription [refilling anti-asthmatic medications without physician visit] [17].
List of anti-asthmatics medications used as an over – the – counter (OTC) in Ethiopia includes [18]:
(1) Ephedrine + Theophylline (in the form of Elixir (6mg + 30mg/5ml), Syrup (2.24% + 0.30%), and Tablet (11mg + 120mg),
(2) Salbutamol (Albuterol) (in the form of Oral Inhalation (aerosol)(0.1mg/dose), Syrup (2mg/5ml), and Tablet (2mg, 4mg, 4mg(s/r)), and
(3) Theophylline + Guaifenesin, 150mg + 90mg; 300mg +180mg (Capsule), 150mg + 90mg/15ml (Elixir), and 150mg + 90mg (Tablet).
2.5. Data Analysis
The data were coded and entered into Epi data 4.2 then exported to the Statistical Package for Social Science (SPSS) 21.0 [21] for analysis. Descriptive analysis was conducted for baseline characteristics of categorical as well as continuous variables; frequency (%) and mean ± standard deviation (SD) were used to present the finding accordingly. Multivariate logistic regression analysis [reported with Adjusted Odd Ratios (AOR) with 95% Confidence Intervals (95% CI) was performed in a backward, step-wise manner, from an initial model which included all explanatory variables with a p-value of <0.25 on bivariate analysis, until a best-fit model was found, to identify factors independently associated with the suboptimal asthma control. P-value ≤0.05 on the final model was considered as a statistically significant associated factor for suboptimal asthma control.
3. RESULTS
3.1. Socio-demographic Characteristics of the Study Population
Of 150 adult asthma patients included in the study, 81 (54.0%) were females, and the mean (± SD) age of the patients was 41.13 ± 12.45 years. More than half of [52.0%] of the study population were rural dwellers (Table 1).
3.2. Clinical Characteristics and Medications Used
Almost all patients (98.7%) had followed up at the OPD chest clinic for more than 1 year. More than one-third of the study participants were taking anti-asthmatic medications without any prescription, while 34.7% had a history of discontinuing the anti-asthmatic medication. One hundred thirty-six (90.7%) patients were reported accessing adequate anti-asthmatic drug information. Among the frequently used anti-asthmatic medications, ICS+SABA accounted highest (42.7%) followed by ICS+LABA (20.7%) and SABA+LAMA+ICS (14.7%). More than two-thirds (75.4%) of patients were taking a combination of two anti-asthmatic medications (Table 2).
3.3. Status of Asthma Control and its Associated Factors
Of 150 adult asthma patients, thirty-nine (26.0%) (95% CI, 19.2%-33.8%) of them had suboptimal asthma control. On multivariate logistic regression, being an urban dweller (AOR=3.70, 95%CI, 1.18-11.59, P=0.025), and not applying proper inhalation technique (AOR=16.23, 95%CI, 1.48-177.76, P=0.022) were associated factors for suboptimal asthma control, while patients having a habit of taking non-prescription drugs (AOR=0.25, 95%CI, 0.08-0.71, P=0.010) had lower odds of suboptimal asthma control (Table 3).
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Sex | Male | 69 | 46.0 |
| Female | 81 | 54.0 | |
| Age | [Mean ± SD] | 43.13 ± 12.45 | years |
| Place of residency | Urban | 72 | 48.0 |
| Rural | 78 | 52.0 | |
| Marital status | Single | 16 | 10.7 |
| Married | 127 | 84.7 | |
| Divorced | 6 | 4.0 | |
| Widowed | 1 | 0.7 | |
| Educational status | Primary school | 64 | 42.7 |
| Secondary school | 8 | 5.3 | |
| College and above | 20 | 13.3 | |
| Can’t write and read | 58 | 38.7 | |
| Job-status | Unemployed | 11 | 7.3 |
| Civil Servant | 20 | 13.3 | |
| Working at a non-governmental organization | 7 | 4.7 | |
| Merchant | 14 | 9.3 | |
| Farmer | 78 | 52.0 | |
| Labor worker | 20 | 13.3 | |
| Variables | Frequency | Percentage [%] | |
|---|---|---|---|
| Comorbidity | Yes | 3 | 2.0 |
| No | 147 | 98.0 | |
| Follow up [>1 year] | Yes | 148 | 98.7 |
| No | 2 | 1.3 | |
| Non-prescription anti-asthmatic medication-taking habit | Yes | 50 | 33.3 |
| No | 100 | 66.0 | |
| Status of smoking | Never used | 134 | 89.3 |
| Past smoker | 12 | 8.0 | |
| Current smoker | 4 | 2.7 | |
| Live with a domestic animal | Yes | 149 | 99.3 |
| No | 1 | 0.7 | |
| History of discontinuing medication | Yes | 52 | 34.7 |
| No | 98 | 65.3 | |
| Adequate drug information | Yes | 136 | 90.7 |
| No | 14 | 9.3 | |
| Anti-asthmatic medications used | SABA+LABA | 18 | 12.0 |
| ICS+SABA | 64 | 42.7 | |
| ICS+LABA | 31 | 20.7 | |
| SABA+LABA+ICS | 15 | 10.0 | |
| SABA+LAMA+ICS | 22 | 14.6 | |
| Variables | Status of asthma control [N=150] | COR[95% CI] | p-value | AOR[95% CI] | p-value | ||
|---|---|---|---|---|---|---|---|
| Good [n=111, 74.0%] | Suboptimal [n=39, 26.0%] | ||||||
| Place of residency | Urban | 50 [33.3] | 22 [14.7] | 1.57[0.75-3.29] | 0.223 | 3.70[1.18-11.59] | 0.025* |
| Rural | 61 [40.7] | 17 [11.3] | 1 | - | 1 | - | |
| Age in years [mean ± SD] | - | 42.3±12.3 | 45.5±12.6 | 1.02[0.99-1.05] | 0.175 | 1.035[.99-1.07] | 0.054 |
| Practicing non-prescription anti-asthmatic drugs taking | Yes | 43 [28.9] | 7 [4.7] | 0.34[0.14-0.85] | 0.021 | 0.25[0.08-0.71] | 0.010* |
| No | 67 [45.0] | 33 [21.5] | 1 | - | 1 | - | |
| Smoking status | Past smoker | 9 [6.0] | 3 [2.0] | 2.94[0.39-21.69] | 0.290 | - | - |
| Current smoker | 2 [1.3] | 2 [1.3] | 0.98[0.25-3.83] | 0.977 | - | - | |
| Never | 100 [66.] | 34 [22.7] | 1 | - | - | - | |
| Discontinuation of anti-asthmatic medication | Yes | 43 [28.7] | 9 [6.0] | 0.47[0.20-1.09] | 0.081 | 0.37[0.14-0.98] | 0.057 |
| No | 68 [45.3] | 30 [20.0] | 1 | - | 1 | - | |
| Educational status | Primary school | 42 [28.0] | 22 [14.7] | 4.71[1.00-22.19] | 0.050 | - | - |
| Secondary school | 6 [4.0] | 2 [1.3] | 3.00[0.34-26.19] | 0.320 | - | - | |
| Can’t write and read | 45[30.0] | 13 [8.7] | 2.60[0.53-12.69] | 0.238 | - | - | |
| College and above | 18[12.0] | 2 [1.3] | 1 | - | - | - | |
| Applying proper inhalation techniques | No | 98 [65.3] | 38 [25.3] | 5.04[0.63-39.8] | 0.125 | 16.23[1.48-177.76] | 0.022* |
| yes | 13 [8.7] | 1 [0.7] | 1 | - | 1 | - | |
4. DISCUSSION
In the current study, 39 [26.0%] adult asthmatic patients had suboptimal asthma control. Being an urban dweller, non-prescription anti-asthmatic medication taking and not applying proper inhalation technique were associated factors of suboptimal asthma control.
Numerous studies across the world showed asthma control to be suboptimal. For instance, of asthma patients, in Europe 53.5% [22]-56.5% [23], United States of America 81.9% [24], Australia 45.7% [25], Thailand 46.5% [26], in Asia 65.3% [27], Europe-America 51.0% [28], Turkey 48.5% [29], and Tunisia 90.0% [30] had suboptimal asthma control. The suboptimal asthma control can be considered as the result of the interaction of the different variables, such as the role of guidelines diffusion and implementation, some disease-related factors (i.e., the presence of common comorbidities in asthma such as Eastroesophageal Reflux Disease (GERD), rhinitis, sleep disturbances and Obstructive Sleep Apnea (OSA) or patient-related factors (i.e., adherence to treatment and coping strategies) [13].
Despite, asthma control status in Africa has not been well studied, a recent study from Cameroun reported 42.0% of the study population had inadequately controlled asthma [31]. Other studies from Nigeria have reported 82.9% [32] inadequately controlled asthma. Democratic Republic of Congo (DRC) 56% [33], the North Africa countries 71.3% [34] and Ethiopia, Addis Ababa 53.3%-75.8% [14, 35] and Jimma 76.1% [36] have reported uncontrolled asthma. The results of the previous reports were higher than the current finding, which might be explained by the previous studies' findings that enrolled large sample size, studied over an extended duration along with different study settings. Therefore, all these factors might be considered favourable to increase the probability of detecting the actual status of asthma control. Another possible explanation might be that patients in the current study were recruited from a chest clinic located in a tertiary center (more pulmonologist avail); it has previously been demonstrated that asthma patients seen by specialists are more likely to be better managed than those followed by non-specialists [37, 38]. Furthermore, advancement in asthma treatment guidelines, as well as its diffusion and implementation over time may also contribute to improvements in asthma treatment outcomes [1, 39].
In the current study, all patients were taking more than one anti-asthmatic drug (combination therapy) and the most frequently used anti-asthmatic medications were ICS+SABA [42.7%] followed by ICS+LABA (20.7%) and SABA+LAMA+ICS (14.7%). However, they differed in comparison with other studies in India [40, 41]. Around 80-92% were taking multi-therapy (≥2drugs), and Methylxanthine (35.5-40%) was the most frequently prescribed drug among anti-asthmatics, followed by β2-agonists (23.9-27%), and corticosteroids (22.6-23%). This difference might be due to the current study conducted in the era of the updated GINA guideline 2019 avail, which recommends that all adults and adolescents with asthma should receive ICS-containing controller treatment to reduce their risk of serious exacerbations and to control symptoms [42]. Another possible reason might be due to differences in adherence to global asthma treatment guidelines across the study setup. On top of routine availability of short-acting bronchodilator anti-asthmatic medications (basically inhaled SABAs) in the current study environment, around one-third of the participants in the current study had the habit of taking non-prescription anti-asthmatic medication. These would justify the high proportion of taking ICS+SABA in this study. On the other hand, theophylline is not routinely recommended for the management of asthma in Ethiopia due to the safety profile [43].
We identified factors associated with suboptimal controlled asthma. Urban dweller asthmatic patients were more than threefold more likely to have suboptimal outcomes than rural dwellers (P=0.025). Exposures relating to environmental and lifestyle changes that originate from the urbanization process have been identified as risk factors for asthma as well as suboptimal control of it, including changes in diet, sedentarism, reductions in childhood infections, dust mites, high levels of vehicle, use of antibiotics, and environmental pollution [44].
Patients taking non-prescription drugs had 25% less likely to have suboptimal asthma control (P=0.010). Non-prescription anti-asthmatic drugs are not actively promoted. Despite this, nonprescription availability would primarily reduce economic barriers like transport cost, physician office visit cost, and better adherence to anti-asthmatic medication by increasing access to the medication [45, 46]. This will, in turn, reduce the probability of developing suboptimal asthma control (or enhance good asthma control).
In our study, asthma patients who were unable to apply the proper inhalation technique were more than sixteen-fold more likely to develop suboptimal outcomes (P=0.022). This might be explained by the proper inhalation technique that can increase medication efficacy, reducing both dose and side effects. On the other hand, deviation from the proper inhalation may result in a decrease in medication efficacy and increase side effects, affecting treatment outcome [47]. Despite the fruitful finding of our work, we acknowledge some limitations that are included in our study relying on physician-diagnosed asthma and the lack of incorporating spirometry-based assessment to assess the status of asthma control. The study also lacked a report on the severity classification of asthma and lacked data on specific non-prescription anti-asthmatic medications used. We were unable to construct a cause-effect relationship due to the cross-sectional study design. Furthermore, the study was single-center, which may limit the generalization of the results to the region and the country.
CONCLUSION
In conclusion, suboptimal asthma control is high among adult asthma patients. Being an urban dweller and not applying proper inhalation techniques increased the likelihood of suboptimal asthma control, while patients having a habit of taking non-prescription drugs had lower odds of suboptimal asthma control. Clinicians/pharmacists have to pay attention to provide adequate anti-asthmatic drug information to their patients. We recommend large sample size studies on the comparative status of asthma control using prescription versus non-prescription anti-asthmatic medication.
LIST OF ABBREVIATIONS
| COPD | = Chronic Obstructive Pulmonary Disease |
| DALYs | = Disability-Adjusted Life Years |
| DRC | = Democratic Republic of Congo |
| JMC | = Jimma Medical Center |
| GERD | = Gastroesophageal Reflux Disease |
| GINA | = Global Initiative for Asthma |
| ICS | = Inhaled Corticosteroids |
| LABA | = Long-Acting Beta-Agonists |
| LAMA | = Long-Acting anti-Muscarinic Agents |
| OPD | = Outpatient Department |
| OSA | = Obstructive Sleep Apnea |
| SABA | = Short-Acting Beta-Agonists |
| WHO | = World Health Organizations |
AUTHORS' CONTRIBUTIONS
The analysis was conceptualized by Mengist Awoke Yizengaw and Kuol Peter Lual. Data collection was managed by Kuol Peter Lual and data analysis was conducted by Mengist Awoke Yizengaw with the support of Kuol Peter Lual. Mengist Awoke Yizengaw drafted the manuscript. Both authors approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance and approval were obtained from the Institutional Review Board [IRB] of Jimma University, under the reference number of SOP131/11.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written consent was obtained from the participant following describing the purpose of the study.
STANDARDS OF REPORTING
The study was conducted in accordance with the STROBE guidelines.
AVAILABILITY OF DATA AND MATERIALS
“The data supporting the findings of the article is available in the repository name of the “data set” submitted online.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Our deepest gratitude extends to Jimma university medical center chest clinic staff members for their cooperation as well as data collectors and patients. Finally, we are indebted to all the staff members at the School of Pharmacy for the immense knowledge impacted during this work.


