All published articles of this journal are available on ScienceDirect.
Different Modalities Used in the Art of Managing Tracheobronchial Foreign Bodies
Abstract
Introduction:
Foreign body aspiration is a commonly encountered and challenging emergency. Foreign body aspiration causes significant morbidity and mortality in the paediatric population. In adults, it is usually encountered in patients with impaired consciousness and in young females using pins to secure their veils. We aimed to analyse the incidence, type and site of foreign body, radiological presentation, complications and different modalities used in managing tracheobronchial foreign bodies (FBs).
Methods:
A prospective single centre cross-sectional study between December 2010 and December 2011 in the Department of Cardiothoracic Surgery at the University of Alexandria, Egypt.
Results:
Seventy-eight patients were included. The age of the patients ranged between 1.3 and 32 years, with a mean of 13.37± 7.67 years. Inorganic FBs were the most common aspirated FBs (66 patients, 84.62%). FBs were more frequently located in the left versus the right bronchial tree (44.9% vs. 43.6%). Rigid bronchoscopic extraction of foreign bodies was the most common modality of extraction and was seen in 60 patients (76.9%), followed by thoracotomy and postural drainage in eight patients each (10.3%). Complications were observed in 12 patients (15.4%). Most of the patients who presented with pin aspiration were teenagers (> 10 – 20 years) and adults (> 20 years). At the same time, nut aspiration was common in children below 10 years.
Conclusion:
The location of FBs in the tracheobronchial tree depends on the patient's age and physical position at the time of aspiration. Rigid bronchoscopy offers better manipulations inside a secured airway and is the preferred method for foreign body removal. If failed, then surgical extraction should be done as soon as possible.
1. INTRODUCTION
Inhaled foreign bodies (FBs) remain a significant cause of morbidity and mortality especially in young children, with a mortality rate approaching 2.5% [1]. The high incidence in children is due to their tendency to explore things by putting them in their mouths. Tracheobronchial FB aspiration is infrequent in adults. Aspiration of FBs in adults can be related to neurological impairment or and alcohol consumption [2]. In Egypt,and other Islamic countries where women wear headscarves, there is a high incidence of inhaled FBs due to the behaviour of placing the pins in their mouth prior to attaching them to their veils [3].
The geometry and chemistry of the inhaled foreign body govern the pathological sequelae. A foreign body that is small and has a smooth surface tends to be well tolerated. Metal, especially iron and steel, produces the least reaction. Vegetable substances such as peanuts and beans produce the most severe inflammation [4]. We herein present our experience in the management of tracheobronchial foreign bodies describing the nature of inhaled foreign bodies and the demographics of patients.
2. CLINICAL RATIONALE FOR THE STUDY
Foreign body aspiration is commonly encountered in the paediatric population and infrequently in adults with impaired consciousness as well as women using pins to secure their veils in Islamic countries. The nature and location of the FBs entail different techniques sand approaches. This study describes the presentation and management of patients with foreign body aspiration in the period between 2010-2011.
3. MATERIALS AND METHODS
Between December 2010 and December 2011, 78 patients with foreign body aspiration presenting to the Department of Cardiothoracic Surgery in Alexandria University Faculty of Medicine were studied. Ethical approval from the Institutional Review Board (IRB) and patients’ consent was obtained prior to the study.
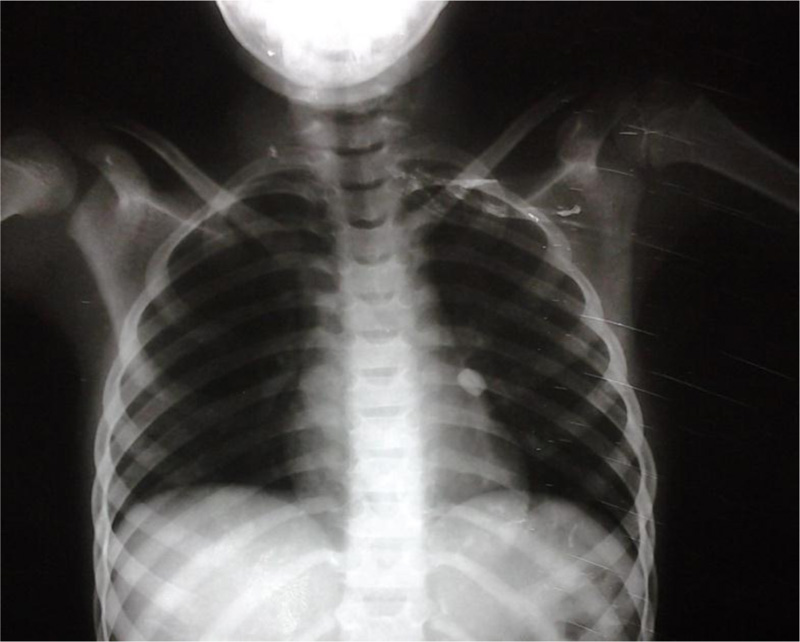
Patients were subjected to clinical assessment by recording vital signs and chest examination. Posteroanterior and lateral chest X-ray films were obtained to assess the presence of the foreign body, its shape, size and effects. Computed tomography scan of the chest was sometimes done with or without virtual bronchoscopy if the data obtained from plain X- rays are still not helpful in doing so.
After confirmation of FB aspiration, patients were admitted and prepared for rigid bronchoscopy to locate the foreign body in the tracheobronchial tree, confirm the data obtained from imaging, evaluate the degree of inflammation or suppuration of the bronchial mucosa, and choose the technique that is necessary for therapeutic measures.
Regarding the technique, the bronchoscope was either used to elevate the epiglottis visualizing the vocal cords or introduced into the trachea under vision. When these maneuvers were unsuccessful, laryngoscopy is done first then the appropriate size bronchoscope is advanced into the trachea.
For organic FBs, the FB forceps were advanced until it lightly touched the FB, the endoscope was then withdrawn a short distance to permit the forceps blades to be opened, and the forceps blades were advanced until the tip passed the equator of the object, then they were closed. The grasp of the forceps was maintained firmly by the fingers of the right hand, while all the traction for withdrawal was made by the left hand. Finally, the forceps holding the FB inside the bronchoscope altogether were removed as one unit. Suction was used to remove secretions from around the FB and sometimes to extract fragmented organic FBs.
For plastic spherical FB, after the failure of extraction using the conventional FB forceps, we used the 7F 80cm Fogarty embolectomy catheter to extract the oval plastic bead. The catheter passed through a central hole in the bead and the balloon was inflated distal to the bead. Finally, the catheter, FB and the endoscope were all removed together as one unit Figs. (1 and 2).


As for sharp metallic FBS, the forceps holding the FB firmly were withdrawn to protect the airways mucosa from being injured during extraction. If the metallic FB could not be grasped by the FB forceps and was seen with its axis parallel to the axis of the bronchus, we performed magnetic extraction using a special magnetic closed FB forceps. The FB (pin) was extracted smoothly without bending or manipulations Fig. (3).
In some patients the removal of a metallic aspirated FB was impossible due to inflammation, marked suppuration of the bronchial mucosa, bronchospasm or inadequate visualization of the FB impaction or distal location. We commenced them on intravenous antibiotics, corticosteroids, frequent nebulizer settings using a beta agonist and performed repeated chest percussion and encouraged coughing as an attempt to try postural drainage. Then we attempted to remove FB after 48-72 hours in the operating room using the bronchoscope with help of biplane fluoroscopy Fig. (4), if the FB was within the reach of the endoscope in the first trail. However, when the FB was situated out of reach of the endoscope, a thoracotomy was done.

In chronic cases, when the whole lung lobe was seen destroyed, we performed a lobectomy via standard postero-lateral thoracotomy incision Fig. (5). In subacute cases, when the lobe was not destroyed with just an atelectatic area seen at the site of the FB, we started locating the exact position of the FB by palpating and milking it towards the periphery. The lung parenchyma and the involved bronchus were incised about 1 cm; the FB was then grasped and extracted using mosquito forceps Fig. (6).
In some cases, when performing thoracotomy for extracting a metallic FB (pin) in an operating room where biplane fluoroscopy was available, we used it to locate the exact position of the FB and grasped it with a Duvall forceps, then performed the bronchotomy procedure.
4. RESULTS
Sixty-five patients were females (83.3%) and 13 were males (16.7%). The age of the patients ranged between 1.3 and 32 years, with a mean of 13.37 ±7.67 years. Twenty-three patients were below 10 years (29.5%), 44 were from 10 to 20 years (56.4%) and 11 were above 20 years (14.1%).
Inorganic objects were the most common FBs aspirated (n=66, 84.62%). The most common inorganic FBs were pins (n=58, 74.4%) followed by plastic objects (n=4, 5.13%). The most common site of foreign body impaction was the right main bronchus (n=15, (19.2%) followed by right lower lobar bronchus. The distribution of studied cases according to circumstances of aspiration, foreign body type and site of impaction FBs is shown in (Table 1).

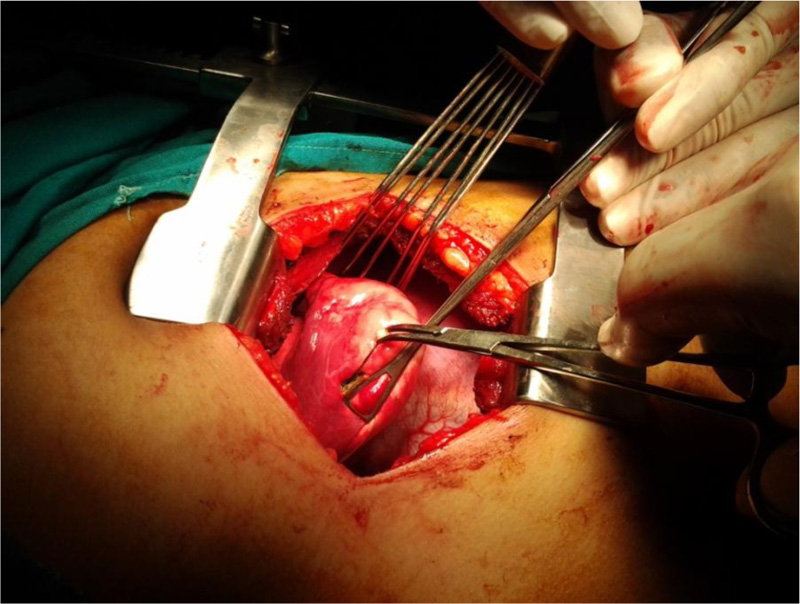
Table 1.
| Number of patients | Percentage | Circumstances of aspiration |
| 31 | 39.7 | Laughing |
| 23 | 29.5 | Talking |
| 13 | 16.7 | Playing |
| 5 | 6.4 | Not known |
| 4 | 5.1 | Improper eating habits |
| 1 | 1.3 | Wearing dental prosthesis |
| 1 | 1.3 | Tooth aspiration |
| Foreign body type | ||
| 58 | 74.4 | Pin |
| 12 | 15.4 | Nut (Squash seed) |
| 2 | 2.6 | Plastic whistle |
| 1 | 1.3 | Plastic bead |
| 1 | 1.3 | Pellet |
| 1 | 1.3 | Small plastic lamp (toy) |
| 1 | 1.3 | Tooth |
| 1 | 1.3 | Dental prosthesis |
| 1 | 1.3 | Sewing needle |
| Site of FB impaction | ||
| 15 | 19.2 | Right Main Bronchus |
| 14 | 17.9 | Right lower lobar bronchus |
| 14 | 17.9 | Left lower lobar bronchus |
| 13 | 16.7 | left Main bronchus |
| 9 | 11.5 | Trachea |
| 7 | 9 | Left upper lobar bronchus |
| 4 | 5.1 | Bronchus intermedius |
| 1 | 1.3 | Lingular bronchus |
| 1 | 1.3 | Right upper lobar bronchus |
Regarding radiological findings, the most frequent finding was radio-opaque FB observed in 64 patients (82.1%), followed by obstructive emphysema in 11 patients (14.1%), consolidation and pulmonary infiltrates in four patients (5.1%) and lung collapse in one patient (1.3%). Normal radiographs were observed in 2 patients (2.6%). Rigid bronchoscopic extraction of the foreign bodies was the most common modality of extraction seen in 60 patients (76.9%). This was followed by thoracotomy and postural drainage observed in eight patients each (10.3%). Flexible bronchoscopic extraction was performed only for two patients (2.6%). The most common complication was failed bronchoscopic extraction (n=10), one patient developed severe bronchospasm and laryngeal oedema that required re-intubation and one patient died from massive bleeding during a trial of rigid bronchoscopic extraction under fluoroscopic guidance (Table 2)
| Number of Patients | Percentage | Symptoms |
| 76 | 97.4 | Cough |
| 44 | 56.4 | Chocking |
| 18 | 23.1 | Breathlessness |
| 16 | 20.5 | Vomiting |
| 14 | 17.9 | Pain |
| 9 | 11.5 | Sputum production |
| 4 | 5.1 | Haemoptysis |
| Signs | ||
| 21 | 29.6 | Wheezes |
| 13 | 16.7 | Crepitations |
| 13 | 16.7 | Diminished air entry |
| 6 | 7.7 | Fever |
| 4 | 5.1 | Tachyapnea & Respiratory distress |
| 3 | 3.8 | Tachycardia |
| 1 | 1.3 | Subcutaneous emphysema |
| Radiological diagnosis (Type of imaging) | ||
| 78 | 100 | Chest X-Ray |
| 2 | 2.5 | CT |
| 1 | 1.3 | Virtual bronchoscopy |
| Radiological findings | ||
| 64 | 82.1 | Radio-opaque foreign body |
| 11 | 14.1 | Hyperinflation (obstructive emphysema) |
| 4 | 5.1 | Consolidation and pulmonary infiltrates |
| 1 | 2.6 | Normal |
| 1 | 1.3 | Collapse |
| Modality of extraction | ||
| 60 | 76.9 | Rigid bronchoscopy |
| 45 | 57.7 | Forceps extraction without fluoroscopy guidance |
| 8 | 10.3 | Magnetic extraction |
| 4 | 5.1 | Suctioning |
| 2 | 2.6 | Forceps extraction (fluoroscopy guided) |
| 1 | 1.3 | Fogarty catheter extraction |
| 8 | 10.3 | Postural drainage and chest percussion |
| 2 | 2.6 | Flexible bronchoscopy |
| 8 | 10.3 | Thoracotomy |
| 6 | 7.7 | Bronchotomy without fluoroscopy guidance |
| 1 | 1.3 | Bronchotomy (fluoroscopic guided) |
| 1 | 1.3 | Lobectomy |
5. DISCUSSION
Foreign body aspiration remains a common but largely preventable problem. It is common in young children due to their tendency to put items in their mouths. In adults, aspiration occurs in cases with impaired consciousness, sedation and orofacial trauma [5]. In Islamic regions, where the considerable number of women wear veils for religious causes, there is a high incidence of accidental aspiration when women tend to place the pins in their mouths while adjusting the veils on their heads [6]. In our study, the median and the mean age were 14 and 13.37, respectively, this is due to the high incidence of headscarf pins aspiration in adolescent girls (63% of the cases).
In our study, the most common aspirated foreign bodies were pins (74.4% of patients), followed by nuts (15.4%). This finding is explained by the higher presentation of females in the sample, who tend to use safety pins in their daily routine.
As regards the site of lodgement of foreign bodies, we found that the majority lodge in the bronchial tree (88.46%), with the remainder in the trachea (11.53%) and none of them lodged in the larynx.
A higher incidence of right-sided foreign bodies (52%) in comparison with left-sided foreign bodies (33%) was reported in most of studies. The exception was a small series in Israel as reported by Cohen S et al. [7-9].
Most patients had chest radiographs. As was reported in 20 studies, only 11% of the FBs were radio-opaque. Chest radiographs were normal in 17% of children with aspirated FBs. The common radiographic abnormalities included localized emphysema and air trapping, atelectasis, infiltrate, and mediastinal shift.
Metallic foreign bodies are easily identified with great accuracy, but their frequency is low, around 10%. When the foreign body is not radiopaque, it is not detected in the radiograph ;however, it could be suspected due to the presence of atelectasis, pneumonitis, air trapping, or mediastinal displacement in the exhaled chest radiograph [7].
In our study, metallic foreign bodies were present in 64 patients (82.1%) comprising a very high incidence compared to other studies. The common radiographic abnormalities due to radiolucent FB aspiration were hyperinflation, atelectasis, infiltrate, and mediastinal shift, which coincide with other studies. We did not report; however, any case with pneumothorax or pneumomediastinum.
AdaletliI et al. stated that computed tomography and virtual bronchoscopy correctly identified all cases of foreign body aspiration. Therefore, some authors suggested that children with a negative CT and virtual bronchoscopy may not require conventional bronchoscopy as a definitive work-up [10].
In our study, virtual bronchoscopy was used in one child presented with non-resolving pneumonia and foreign body aspiration was a possible diagnosis. A FB was detected in the bronchus intermedius. Rigid bronchoscopy was done, the diagnosis was confirmed, and the FB was successfully extracted.
In our study, we removed the FBs by bronchoscopy (both types) in 79.5% of the cases. The rigid bronchoscopy was the main technique used in the removal of aspirated FBs (76.9% of the cases), as described in the literature. Rigid bronchoscopy, therefore, constitutes an important tool in the handling of airways in children, increasing the ventilation safety, and handling during the procedure [11].
We observed a high incidence of surgical treatments. Thoracotomy was performed in 8 patients (10.3%). There main factors explaining a large number of thoracotomies are parenchymal sequelae following recurrent infections due to delayed diagnosis in some cases, the special nature of some foreign bodies and the fact that our hospital is a thoracic surgery reference centre for the western north of Egypt.
Major iatrogenic complications were specified in 21 studies with 9437 children with aspirated foreign bodies. These complications included severe laryngeal oedema or bronchospasm requiring tracheotomy or re-intubation, pneumothorax, pneumomediastinum, cardiac arrest, tracheal or bronchial laceration, and hypoxic brain damage. These major complications occurred in 91 of these 9437children (0.96%). Other reported serious complications included infection, bleeding, and failed bronchoscopic removal that necessitated thoracotomy or tracheotomy. Mortality data were obtained from 26 articles with 43 deaths among 10,236 children (0.42%) with aspirated foreign bodies. Twenty-five deaths occurred in the 5 largest series with 5927 children (0.42%) [12]. Compared to the major iatrogenic complications reported, we reported one child developing severe bronchospasm and laryngeal oedema that required re-intubation (1.28%); we did not report any case of pneumothorax, pneumomediastinum, cardiac arrest, tracheal or bronchial laceration, or hypoxic brain damage. Thoracotomy was performed in 10 cases (12.8%) after failed bronchoscopic extraction.
The mortality rate in our cohort was (1.28%) which is slightly higher compared to other studies. The cause of death was the massive tracheobronchial bleeding following a bronchoscopic trial of extraction of a pin with fluoroscopic guidance. We did not report any fatalities due to acute cyanosis or respiratory distress. This can be explained by the higher incidence of pin aspiration in our study compared to the other studies and that sharp metallic pins are more liable to cause bleeding during their extraction compared to other types of FBs.
CONCLUSION
Tracheobronchial foreign bodies will always remain a challenging area of management. The nature, geometry, site, timing of presentation and patient age largely impact the procedure's outcome and success. Bronchoscopy remains the first line of management, however, more complicated cases will require certain modifications of the procedure to overcome the complexity of the presentation. As a last resort, surgery might be required to extract the foreign body. The overall safety of the procedure has increasingly improved in the past decades due to the advance of surgical instruments and the increased cumulative experience of surgeons.
Tracheobronchial foreign bodies are commonly encountered in clinical practice, yet challenging due to the variety and timing of the presentation as well as the position of foreign bodies. Tracheo-bronchial FBs are more common in paediatric population, however, in Islamic countries accidental pin aspiration is frequently encountered in young women due to the use of pins to secure their veils. Different techniques and modalities of management are applied to improve the outcomes and minimize the surgical intervention. Continuous improvement of intervention and techniques is critical because the population requiring the intervention is expanding and the nature of the aspirated materials is changing over time.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional review board (IRB).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. The reported experiments on humans are in accordance with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all individual participants included in the study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [H.M.H], on special request.
FUNDING
This publication was prepared without any external sources of funding.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
Declared none.


