All published articles of this journal are available on ScienceDirect.
IgE Mediated Wheat Allergy Associated with Resistant and Severe Forms of Allergic Conjunctivitis
Abstract
Objective:
This study aimed to determine the prevalence and criteria of wheat allergy (WA) among patients with resistant allergic conjunctivitis (AC).
Methods:
A prospective comparative study was conducted on 100 patients with resistant AC. Skin prick-tests (SPTs), total and sIgE against a panel of inhalant and food allergens were performed in all patients’ sera. They were divided into 2 groups according to skin prick test (SPT) and specific IgE (sIgE) level, namely the wheat sensitive group (WSG) and wheat tolerant group (WTG). Total ocular symptom scores (TOSS) and 4-point sign scales were correlated for both groups.
Results:
Ten patients out of 100 with IgE-mediated resistant AC were wheat sensitive, and the other 90 were wheat tolerant patients. WSG included patients of significantly younger age. Positive family history of atopy was proven in 100% of WSG vs. 67% of WTG. A significantly higher frequency of multiorgan allergy was detected in 100% of WSG vs. 20% in WTG (P = 0.0001). Thirty (30%) of WSG had associated allergic rhinitis (AR) and bronchial asthma (BA). Another 30% had an associated AR only, 10% had an associated BA only, and another 20% had an associated skin allergy. TOSS, 4- point sign scale, and total IgE level were significantly higher in WSG.
Conclusion:
This study provides novel evidence that wheat allergy is responsible for some severe forms of AC.
1. INTRODUCTION
Wheat is the most popular grain worldwide. Flour and bran are used in the production of many food products, such as bread, breakfast cereals, and pasta. Being a binding agent, wheat is added to desserts, cream, and ice cream. Starch is used for coating pills and roasted coffee grains, as well as in a variety of pharmaceuticals, cosmetics, and chemical industries [1, 2].
Its use is so widespread that people suffering from gluten-related disorders face difficulty avoiding it [2]. Wheat allergy, as a sIgE- mediated reaction, is a complex disease due to the many allergenic components in wheat [3, 4]. These patients tend to have severe reactions compared to reactions from other kinds of food, such as eggs and cow milk [5].
Hypersensitivity IgE-mediated reactions to wheat can be due to either ingestion or inhalation (food allergy or respiratory allergy) [6]. Wheat can also cause contact allergy when using cosmetics that contain hydrolyzed wheat protein [7, 8]. Allergic conjunctivitis can be caused by various allergens, such as mixed pollens, house dust, mites, hay dust, feather, and animal dander [9]. The natural history of IgE-mediated WA has been infrequently reported and studied [10]. However, little information is available about the relationship between wheat and allergic conjunctivitis. The diagnosis of the condition can be tricky because wheat is present in so many different foods. Therefore, a high index of suspicion is required [11].
Accordingly, the aim of the present study is to investigate the prevalence of wheat allergy among patients with resistant AC, when to suspect it, how to confirm the diagnosis, and the relationship between wheat allergy and the severity of the AC.
2. MATERIALS AND METHODS
2.1. Study Population and Design
A prospective comparative case series study was conducted in cooperation with the Ophthalmology Department and Allergy Clinics of the Respiratory Medicine Department, Sohag University. Before undertaking the study, all patients were informed of the potential risks and benefits of skin testing and signed written informed consent forms to participate. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Local Ethical Committee of Sohag University Hospitals.
Patients included in the study were those with resistant AC (resistant to steroid sparing topical or systemic medications) with high total serum IgE level as a screening test to confirm IgE mediated hypersensitivity. Those patients were referred to allergy clinics for allergen identification by SPT and sIgE level.
Patients on long-term systemic steroids or systemic antihistaminics were excluded. Immuno-compromised patients, patients with a parasitic infestation and skin diseases precluding SPT, and pregnant women were also excluded.
The study was conducted on 100 patients (who met the inclusion criteria). Patients were divided into 2 groups according to the result of SPT and specific IgE level: sensitive wheat group (WSG) if one of both tests were positive for the wheat and wheat tolerant group (WTG) if both tests were negative for wheat allergen.
All patients underwent a complete ophthalmic examination, including recording of symptoms, slit-lamp biomicroscopy, and fundus examination. Anterior-segment photographs were taken. Total ocular symptoms score [9] was used for grading the severity of symptoms, while a 4-point sign scale [12] was used for grading the signs by one examiner.
2.2. Allergometric Evaluation
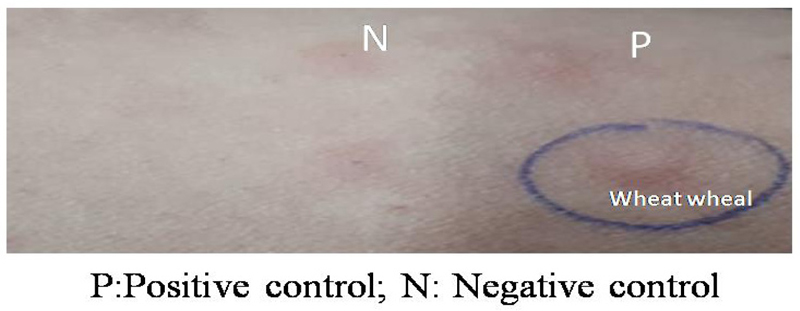
Skin prick-tests (SPTs) were performed on all patients using commercial extracts for a standardized panel of inhalant and food allergens (Fig. 1).
In addition, total IgE was measured by enzyme-linked immunosorbent assay (ELISA), and sIgE levels against a panel of inhalant and food allergens were determined in all patients’ sera by a commercially available kit (immunoblot EUROLINE, Germany) which consisted of 34 allergens. sIgE levels greater than 0.35 kU/L were considered positive.
2.3. Statistical Analysis
SPSS ver. 20 (SPSS Inc., Chicago, IL, USA) were used for statistical analyses. Student's t-test was used to analyze the difference between the 2 groups. Z test was used to compare between 2 proportions. Spearman or Pearson method was used to test correlation. A p-value of <0.05 is considered statistically significant.
3. RESULTS
Patients’ demographics and baseline characteristics are shown in Table 1.
| Characteristic | WSG | WTG | P value |
|---|---|---|---|
| Age (yr) | 22.8±13.2 | 34.22±12.5 | 0.033 |
| Sex (male/female) | 70% | 57% | 0.61 |
| TOSS | 88.98±12.99 | 68.11±22.24 | 0.012 |
| The 4-point sign scale | 2.50±0.53 | 1.17±0.79 | P=.000 |
| Family history of allergy | 10/10 | 12/18 | 0.007 |
| Mean wheal size (mm) | 7.40±2.011 | 3.72±0.57 | 0.000 |
| Mean Total IgE (mean, kU/L) | 333.4±336.4 | 134.32±128.44 | 0.033 |
| Patient No. | Age | Sex | FH | TOSS | Symptoms | FA/aeroallergens | Wheal size (mm) |
Total IgE (kUA/l) |
Specific IgE (kUA/l) |
|---|---|---|---|---|---|---|---|---|---|
| P1 | 7 | F | + | 18.75 | AC-GI | Wheat flour | 7 | 760 | 23 |
| P2 | 18 | F | + | 83.5 | AC-BA- AR | Wheat flour | 2.5 | 530 | 20 |
| P3 | 5 | M | + | 81.25 | AC-BA- AR | Wheat flour | 5 | 900 | 0.32 |
| P4 | 14 | F | + | 60 | AC-BA- AR | Wheat flour+G pollens | 9 | 240 | 9 |
| P5 | 24 | M | + | 31.25 | AC-AR | Wheat flour | 1.5 | 710 | 19 |
| P6 | 9 | M | + | 67.50 | AC-Urticaria | Wheat flour | 7 | 420 | 0.21 |
| P7 | 6 | M | + | 75 | AC-Urticaria | Wheat flour | 5 | 570 | 21 |
| P8 | 12 | F | + | 18.75 | AC-BA | Wheat flour+ G pollens | 9 | 1320 | 27 |
| P9 | 30 | F | + | 55.75 | AC-AR | Wheat flour | 9 | 310 | 11 |
| P10 | 10 | F | + | 88.25 | AC-AR | Wheat flour | 2 | 100 | 6 |
3.1. WSG; Wheat Sensitive Group, WTG; Wheat Tolerant Group, TOSS; Total Ocular Symptoms Score
Ten patients (10%) out of 100 patients with IgE-mediated resistant AC were wheat sensitive, and the other 90 patients were wheat tolerant. The mean age was 22.8±13.2 and 34.22±12.5 for WSG and WTG, respectively; WSG included patients of significantly younger age (P = 0.033). The female gender predominated in WSG than in WTG without a significant difference (P=0.61). Family history of atopy was proven in 100% of WSG vs. 67% of WTG, with a statistically significant difference between both groups (P=0.007).
TOSS was significantly higher in WSG (88.98±12.99 vs. 68.11±22.24 in WTG P=0.012). The 4-point sign scale was significantly higher in WSG (2.50±0.53 vs. 1.17±0.79 in WTG P=.000). Total IgE level was significantly higher in WSG (333.4±336.4) than in WTG (134.32±128.44 P=0.33). Considering SPT, the mean wheal diameter for allergen extract was significantly higher in WSG (7.40±2.011mm) than in WTG (3.72±0.57mm) (P=0.000).
In WSG, both SPT and SIgE were +ve for wheat flour allergen in 50% of wheat-sensitive patients. Positive SIgE but –ve SPT results were found in 30% of WSG, whereas +ve SPT and –ve SIgE results were detected in 20% of WSG (Table 2).
A significantly higher frequency of multiorgan allergy was detected in 100% of WSG vs. 20% in WTG; P= 0.0001. Thirty (30%) patients in WSG had associated allergic rhinitis (AR) and bronchial asthma (BA). Another 30% had an associated AR only, 10% had an associated BA only, and another 20% had an associated skin allergy (Table 2).
4. DISCUSSION
Wheat allergy is an allergic reaction that is mainly induced by eating food products that contain wheat. Diagnosis can be challenging because wheat is present in many different foods [11]. Little information is available about the relationship between wheat allergy and allergic conjunctivitis.
Although wheat allergy is rare, it is one of the most widespread food allergies. The patterns and prevalence of food allergy are highly variable in different parts of the world, which is attributed to a complex interplay of environmental, genetic, and epigenetic factors [13]. Prevalence of wheat allergy, in general, was found to be 0.21% in one study [14] and ranged from 0.2-1.3% in other studies [15, 16].
Our study revealed an incidence of 10% of wheat allergy among patients with resistant AC. Wheat allergy is considered resistant as the triggering allergen is present in many products; therefore, it is difficult for the patient to correlate between exposure to a certain product and the development of symptoms. Moreover, symptoms will not resolve except after the stoppage of exposure to the triggering allergen.
Regarding the age difference in the study, patients in WSG had a significantly younger age than WTG. This is consistent with previous reports that young age groups have a higher prevalence of wheat allergies compared to adults because their immune and digestive systems have not yet matured, and this age group is more likely to develop this type of allergy if wheat is introduced after 6 months of birth [11, 17].
Furthermore, the study reported a higher frequency of female gender in WSG than in WTG (though insignificant). It was reported previously that female dominance is a significant factor in terms of food allergy [18].
The study revealed a positive family history of allergy in 100% of WSG vs. 67% of WTG. A positive family history of allergy was reported to be an important risk factor for wheat allergy, and these patients tend to have a high atopic potential [19].

The protocol for treating AC in our institutions is to start with short-term steroid eye drops to control acute symptoms, then continue on maintenance therapy with any steroid-sparing agents. If symptoms are persistent or the frequency of steroid-containing eye drops increases, AC is considered resistant, indicating the presence of a triggering allergen highly probable. The patient is then referred to a total serum IgE level assessment as a screening test for IgE-mediated allergy; if high levels are found, then the patient is referred to allergy clinics for allergen identification by SPT and specific IgE level.
The study revealed significantly higher total IgE levels in WSG than in WTG. Allergy sensitization mediated by IgE is the basis of allergic diseases, and elevated total IgE is frequently included as a diagnostic criterion for allergic diseases. Total IgE levels are not elevated only in allergic disorders but also in parasitic diseases and in a specific immune deficiency termed hyper IgE syndrome; both were excluded in this study. Low total IgE indicates a low probability of specific IgE sensitization [20]. Skin prick testing is an essential procedure to confirm sensitization in IgE-mediated allergy in subjects with rhinoconjunctivitis, urticaria, atopic eczema, asthma, anaphylaxis, and drug and food allergy [21]. Specific IgE is integral to the pathogenesis of allergic disorders, and it is crucial to detect the causal allergens in AC to prevent and treat the disease [22].
The study revealed that both SPT and S IgE were +ve for wheat flour allergen in 50% of wheat-sensitive patients. Positive S IgE but –ve SPT results were found in 30% of WSG, whereas +ve SPT and –ve sIgE results were detected in 20% of WSG.
This disagreement between the results of SPT and S IgE levels could explain that the immune response is different in the blood and the skin. Schoos et al. [23] showed substantial discordance between SPT and specific IgE results, suggesting that the two testing methods complement each other and cannot be used interchangeably; if only one type of testing is performed, a substantial number of allergic sensitizations may be missed [24].
The study revealed the presence of a significantly higher frequency of multiorgan allergy in WSG (100%) vs. 20% in WTG. Allergic multiorgan disease triggered by wheat flour allergen in the form of rhinoconjunctivitis and asthma was previously reported. Symptoms developed in the form of watery eyes, itching, sneezing, nasal stuffiness and rhinorrhea [25]. Another study reported a combination of allergic rhinoconjunctivitis, asthma and urticarial from wheat flour sensitization. This sensitization tends to disappear with age [26].
Recognition of such a form of allergy is very important because the improvement of symptoms will be significantly noticeable if the patient refrains from being exposed to foods containing wheat flour (Fig. 2), replacing wheat flour with corn flour and managing the condition by allergen immunotherapy.
CONCLUSION
From this study, we concluded that if AC is IgE mediated, resistant, and in a severe form with symptoms in a young patient having a positive family history of atopy and multiorgan allergy, wheat-mediated AC is highly probable. Further studies are necessary in order to conclude a causal association between wheat flour sensitization and AC.
LIST OF ABBREVIATIONS
| SPTs | = Skin Prick-tests |
| WSG | = Wheat Sensitive Group |
| WTG | = Wheat Tolerant Group |
| BA | = Bronchial Asthma |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Local Ethical Committee of Sohag University hospitals, Egypt (IBR: Soh-Med-21-11-30).
HUMAN AND ANIMAL RIGHTS
No animals were used in the studies that are the basis of this research. This research was conducted on humans in accordance with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
The consent to publish these findings and images was taken from the patients.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS:
The data supporting the findings of the article are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


