All published articles of this journal are available on ScienceDirect.
Precision in Diagnosing and Classifying COPD: Comparison of Historical Height with Current Height and Arm Span to Predict FEV1
Abstract
Background:
Measured reductions in lung function, as a result of COPD, use a measured current value and make comparisons to a determined ‘normal’ value arrived at using a regression equation based upon a patients height. Osteoporosis is a recognised co-morbidity in patients with chronic obstructive pulmonary disease (COPD) and may cause excessive height loss resulting in the ‘normal’ values and disease progression being under-estimated.
Purpose:
The aim of the study was to examine the height variation in a cohort of COPD patients and controls over a 7-8 years period and evaluate its impact on estimates of lung function and hence COPD progression.
Methods:
In 1999-2002 we studied a cohort of primary care patients in Sunderland, UK with and without COPD and reexamined 104 (56 male) during 2007-2009. We calculated FEV1% predicted for actual and estimated height (armspan/1.03 and armspan/1.01 in males and females respectively).
Results:
In 1999-2002 the subjects were aged 62.6 ± 9.4 years, BMI was 26.4± 4.7 kg/m2, predicted FEV1 was 59.0 ±16.0, and mean actual height was 167.3±8.9cm. The actual height changed significantly (p<0.001) by 2cms over time in both genders. Whilst the overall classifications of the cohort did not change significantly when armspan was used to determine height and hence normal lung volume, individual cases did move to a classification of higher severity.
Conclusions:
The study suggests that current measured height may underestimate the degree of impairment of FEV1 and hence progression of COPD. The use of height, derived from armspan, may give a more accurate measure of ‘normal’ lung volumes and hence the degree of impairment.
1. INTRODUCTION
The diagnosis of COPD, chronic obstructive pulmonary disease, currently depends on demonstrating limitations of airflow, using spirometry, the gold standard method for obstructive disease of the airways. A diagnosis of COPD is normally made if the ratio of the forced expiratory volume in the first second (FEV1) to forced vital capacity (FVC) is below 0.70 (Global Initiative for Obstructive Lung Disease – GOLD, 2010) [1].
Impairment of FEV1 has also been utilised to classify the severity of airflow obstruction for COPD, in a range of guidelines, including those recommended by the National Institute of Clinical Excellence (NICE) in the UK [2]. Impairment of FEV1 is determined by making reference to predicted (normal) volumes. As spirometric values are dependant on the size of the lungs, which is in turn directly related to height, gender, age and ethnic origin [3] the predicted normal value for lung capacity is determined using measures for these variables. One regression equation that is commonly used is that proposed in the European Respiratory Society (ERS) guidelines [4].
For Males: PREDICTED FEV1= (4.30 x height) – (0.029 x age - 2.49)
For Females: PREDICTED FEV1= (3.95 x height) – (0.025 x age - 2.60)
However, some of these variables, including height may be affected by other factors including osteoporosis and this will confound the interpretation of comparisons made to a predicted normal value for lung capacity that has been determined based upon a patients’ height.
In terms of height Sorkin et al. [5] found that in healthy Caucasians a longitudinal decline in height, with aging, becomes apparent from the age of 40 years. An initial rate of decline of 1cm per year accelerates after the age of 60 years with women losing more height than men. However, Capderou et al., (2011) [6] in a large single centre study comparing historic height with current measured height concluded that significant height loss becomes important after the age of 70. In patients with COPD height loss may occur at an earlier age due to the high prevalence of osteoporosis in smokers [7, 8]. Osteoporosis is also a recognised complication of regular treatment with oral corticosteroids which are often used to treat exacerbations in COPD [9, 10]. Although there is little systemic absorption of inhaled corticosteroids some concern exists that they might increase the risk of osteoporosis [11, 12]. Hence height may not be the most accurate measure to use, to determine predicted ‘normal’ lung volume in patients suffering from COPD. Using current height to determine the predicted values of FEV1 may mean that the degree of impairment of FEV1 is subject to confounding particularly in an elderly population.
This paper has therefore considered the use of armspan as an alternative measure for the estimation of height and in the prediction of ‘normal’ lung volume. Armspan is quick and easy to measure, is low cost and a useful alternative when standing height is difficult to measure such as in patients with disabilities who cannot stand, bedridden patients and those with bony deformities [7-13].
The research was carried out using a cohort of COPD patients recruited in a primary care setting in the North East of England. Members of the cohort were first examined in 1999-2002. The second examination occurred in 2007-2008.
2. METHODS
In the study reported here the cohort was first evaluated between September 1999 and December 2002, when patients with suspected COPD, attending primary care asthma clinics, were identified by performing spirometry according to the British Thoracic Society guidelines (BTS) [14].
Patients were classified as having COPD utilising the absolute post-bronchodilator FEV1/FVC ratio ≤ 0.7. Exclusion criteria were: FEV1/FVC >0.7; age <40 years and a clear diagnosis of asthma based on BTS criteria of an increment over baseline FEV1 of more than 15% and more than 200mls with the bronchodilator and patient with any obvious bony deformity that may alter armspan or height measurements.
Patients in the non COPD control group were classified as those with FEV1% predicted values of >80% and with no symptomatic evidence of obstructive disease such as cough and shortness of breath.
Height was recorded using a single stadiometer without shoes and arm span was measured. Armspan is defined as the maximum distance from the tip of the middle finger of one hand to the tip of the same finger of the other hand with outstretched arms and the subject standing erect. Spirometry (Vitalograph 2120); before and after bronchodilatation was also undertaken.
FEV1% predicted was determined for measured height and for estimated height based upon armspan (armspan/1.03 and armspan/1.01 in males and females respectively) [15].
In 2007-2008 survivors from this cohort were asked to attend for review.
Sunderland Local Research Ethics Committee approved this study.
Statistical Analysis
The non-parametric Spearman correlation coefficient was calculated to describe the relationships between the continuous variables that were not normally distributed. A two sample t test was used to measure the difference of height and FEV1 predicted values in males and females and paired t test was used to explore the height loss measured 7-8 years apart. ANOVA was employed to examine the distribution of height loss in different age range quartiles.
A chi square test was used to evaluate the significance of the movement of individuals to a different stage classification of COPD (GOLD) dependent on whether their ‘normal’ lung capacity was determined from their measured height or their armspan.
The data analysis was carried out using SPSS 17.0.
3. RESULTS
From the survivors of the original cohort 104 patients with COPD and 42 without COPD attended for review in 2007-2008, Table 1 presents their demographic characteristics.
Demographics of the Cohort According to Gender in 1999-2002
| COPD | Non COPD (Controls) | |||
|---|---|---|---|---|
| Male N=56 | Female N=48 | Male N=19 | Female N=23 | |
| Age | 62.7 ± 9.6 | 61.7± 8.8 | 61.0± 10.0 | 57.2± 8.7 |
| Height (cm) 1999-2002 | 172.7 ± 6.4 | 161.3 ± 7.4 | 172.4 ± 5.9 | 158.3 ± 5.6 |
| Height (cm) 2007-2008 | 170.7 ± 5.8 | 159.4 ± 7.4 | 170.6 ± 5.8 | 157.5 ± 6.6 |
| Armspan (cm) | 177.3±7.8 | 162.8±8.6 | 175.6±7.8 | 161.8±6.2 |
| Height change 1999-2008 | 2.0±2.3 | 1.8±3.5 | 1.7±2.2 | 0.8±2.9 |
| Armspan to height ratio (1999-2002) | 1.03±0.02 | 1.01±0.03 | 1.03±0.02 | 1.02±0.03 |
| Armspan to height ratio (2007-2008) | 1.04±0.03 | 1.03±0.03 | 1.04±0.01 | 1.03±0.03 |
| Pack years | 37.0 ± 13.0 | 36.5 ± 14.8 | 23.5 ± 14.2 | 34.5 ± 7.1 |
| FEV1 | 1.64 ± 0.58 | 1.46 ± 0.48 | 3.00 ± 0.53 | 2.09 ± 0.35 |
| FEV1 loss/year | 0.11±0.002 | 0.11±0.004 | 0.10±0.002 | 0.11±0.002 |
| FEV1%Pred (1999-2002) (Actual height) | 53.0 ± 18.0 | 65.1 ± 14.7 | 95.2 ± 13.0 | 95.8 ± 11.1 |
| FEV1%Pred (1999-2002) (Estimated height) | 53.6 ± 18.2 | 66.0 ± 15.9 | 95.3 ± 13.2 | 91.1 ± 11.1 |
| FEV1%Pred (2007-2008) (Actual height) | 53.3± 17.2 | 57.4 ±16.2 | 97.7 ±10.2 | 96.3 ± 12.0 |
| FEV1%Pred (2007-2008) (Estimated height) | 52.1 ± 16.8 | 55.7 ± 17.7 | 97.6 ± 10.2 | 90.4 ± 13.1 |
| MRC (1-5) | 2.4 ± 0.9 | 2.2 ± 0.8 | 2.0 ± 1.0 | 2.2 ± 0.7 |
| Smoking Status | Current: 20 Exsmokers: 25 Nonsmokers: 11 |
Current: 19 Exsmokers: 19 Nonsmokers: 10 |
Current: 11 Exsmokers: 06 Nonsmokers: 2 |
Current: 10 Exsmokers: 6 Nonsmokers: 7 |
| Passive smoking (yrs) | 39.6 ± 21.4 | 37.1 ± 20.8 | 12.8 ± 16.5 | 36.2 ± 18.8 |
Definition of abbreviations= BMI=Body mass index; FEV1 (% Predicted) =forced expiratory volume in one second predicted for age and sex; FEV1/FVC (%Predicted) =forced expiratory ratio (as predicted); BOD=BMI, airway Obstruction, MRC Dyspnoea score, M=metres; L=litres; MRC=Medical Research Council Dyspnoea Score.
Influence of Calculating FEV1% Predicted from Actual Height and Estimated Height on Severity Classification in COPD Patients
| GOLD Classification | |||
|---|---|---|---|
| 1999-2002 | Measured FEV1 (Measured Height) | Estimated FEV1 % (Calculated Height) | p Value |
| Stage I | n=04 | n=11 | NS |
| Stage II | n=63 | n=57 | |
| Stage III | n=25 | n=24 | |
| Stage IV | n=08 | n=08 | |
| GOLD Classification | |||
| 2007-2008 | Measured FEV1 % (Measured Height) | Estimated FEV1 % (Calculated Height) | p Value |
| Stage I | n=18 | n=18 | NS |
| Stage II | n=44 | n=43 | |
| Stage III | n=33 | n=32 | |
| Stage IV | n=05 | n=7 | |
All members of the COPD cohort showed a significant loss in measured height, mean 2 cm from 1999-2002 to 2007-2008. This can also be seen in Fig. (1) however this difference in height is not shown when height is determined using armspan.
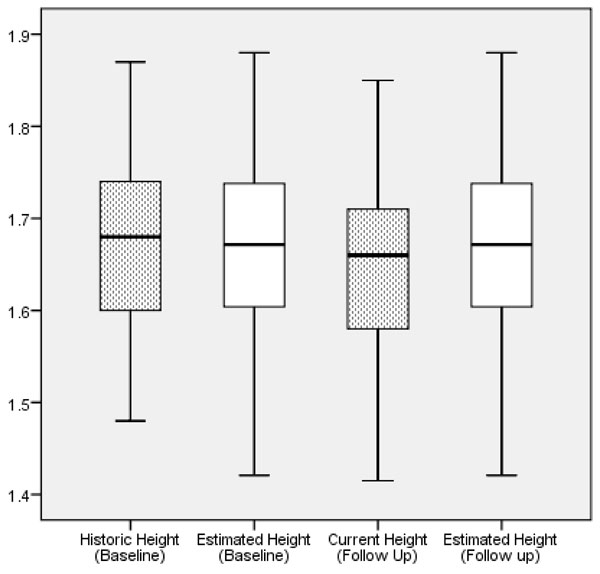
Height variation over time at baseline and followup in study Subjects (All measuremtns were recorded in meters).
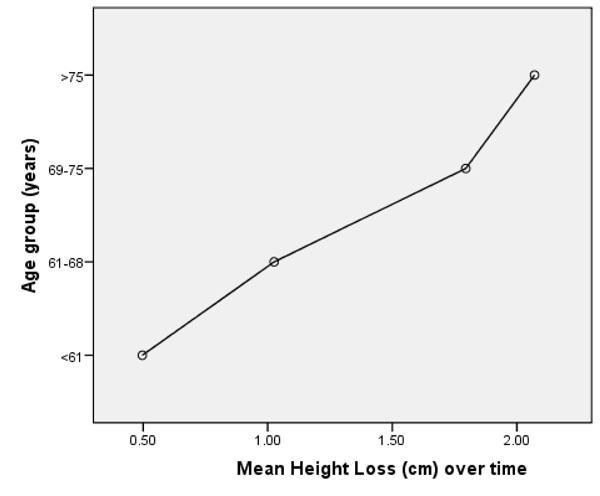
Mean Measured Height Loss overtime (1999/2002- 2007/2008) in different age groups.
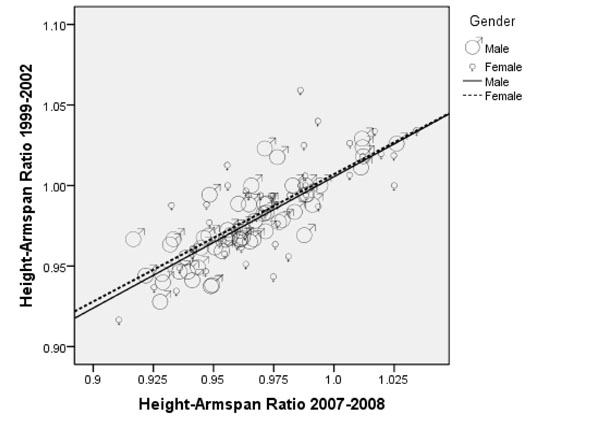
Relationship of Height –Armspan ratio overtime (R2=0.639 in men and 0.575 in women).
Fig. (2) shows that for the cohort, loss of height, increased with age. This loss of height with age is also reflected in the change in armspan to height ratio (Fig. 3) although the results here are more variable.
FEV1% predicted in 2007/8 was significantly (p<0.001) lower when using height determined from armspan – 53.3±17.2% against 52.1 ±16.8% in males and 57.5±16.1 vs 55.7±17.7 in females within the COPD group. However, this difference was only found with the female members of the control cohort.
Table 2 shows the distribution of patients classified according to GOLD criteria in both 19992-2002 and 2007-2008. There was no significant movement between stages as a result of recalculating FEV1% predicted from height estimated from armspan. Whilst this would suggest that there is no need to change the management plan and/or prescriptions for the group overall there will be a significant impact upon those individuals whose classification does change.
DISCUSSION
The accurate classification of COPD is important in that strategies need to be developed for the management of these patients. Therefore if impairment of FEV1 is to be used to classify the stage of disease progression there is a need for accurate predictions to be made for normal lung volumes. These are currently calculated using a regression equation in which current height is one of the variables. However, current height can be confounded by a number of other factors including osteoporosis.
In this study we have shown that patients both those with confirmed COPD and the controls exhibit a significant reduction in mean height of 2cm over a median period of observation of about 8 years. This variation of height in turn influences the predicted values of lung function, calculated to diagnose and classify the stages of COPD, thus underestimating the degree of severity in these patients. The reduction of standing height was more significant in female subjects suggestive of postmenopausal degenerative bony changes in women [16]. This is important as more females are now reporting with COPD.
It is an established problem that standing height loss occurs in elderly people and this is supported by our data (Fig. 2) which shows the mean height loss in different age groups over time. The underlying causes that are responsible for height reduction may include narrowing of vertebral space, age related vertebral fractures mainly due to osteoporosis, regular use of corticosteroid, female sex and lower body weight [19,20].
Armspan has traditionally been used to estimate predicted lung volumes in pulmonary function laboratories especially when the subjects have a spinal deformity or are unable to stand. Armspan is correlated with height and the normal phenomenon is for armspan to slightly exceed height. A number of studies have examined this relationship [13,17,18] and to estimate height from armspan measurements we chose ratios of 1.03 and 1.01 in men and women respectively as appropriate for a Caucasian population [13].
The information presented here shows that the calculated height measured by armspan is similar when estimated over time. However, the standing heights, measured using a stadiometer, are different at baseline and follow up (Fig. 1) indicating a possible under- estimation of normal lung volume if measured height is used to calculated FEV1. If this is the case the severity of COPD progression would be underestimated.
The conclusion that can be reached from these results is that the use of current height will mean that COPD progression is underestimated if measured height is used. The use of armspan to determine height and hence normal lung volume will give a more accurate measure of the impairment of lung function and hence COPD progression.
There are some limitations to the study. The number of subjects both in the COPD and control groups is low however it was possible to demonstrate the impact of height loss across the cohort. Furthermore, historical heights were measured by the clinical staff in their local clinical settings in contrast to the work of Kjensli and colleagues [21]. Kjensli and colleagues reviewed whether height reduction influences interpretation of lung function in COPD patients. However they used the highest remembered height and compared this with current height. They showed that the spirometric values were influenced by height losses of greater than 5.9 cm. This was especially true for those with a low FEV1.
Future longitudinal studies are needed in order to validate our finding with a larger number of subjects.
ACKNOWLEDGEMENTS
The authors would like to thank all patients who participated in the study. The author would also like to thank Higher Education Commission, Pakistan and City Hospitals Sunderland, UK Research Grants to provide financial support to carry out this study.
CONFLICT OF INTEREST
None of the authors of the above manuscript (Dr. Khalid A. Ansari, Dr. N.P. Keaney, Dr. Monica Price, Dr. Joan Munby, Andrea Kay, Ian Taylor, and Dr. Kathryn King) has received fees or funds that might appear to affect their ability to present or review data objectively or serving as a speaker, consultant or an advisory board member in relation to the manuscript aims and objectives.
None of the authors of the above manuscript (Dr. Khalid A. Ansari, Dr. N.P. Keaney, Dr. Monica Price, Dr. Joan Munby, Andrea Kay, Ian Taylor, and Dr. Kathryn King) has any conflict of interest which may arise from being named as an author on the manuscript.


